Heme biosynthesis and Disorder, Types of porphyrias, Fate of RBs and Catabolism of Hemoglobin
Heme consists of a ringlike organic compound known as porphyrin and attached to an iron atom, It is the iron atom that reversibly binds oxygen as the blood travels between the lungs & the tissues. Steps of heme synthesis are Synthesis of δ-aminolevulinic acid, Synthesis of porphobilinogen, Synthesis of uroporphyrinogen, Synthesis of coproporphyrinogen, Synthesis of protoporphyrinogen III, protoporphyrin and heme.
Heme biosynthesis
Heme is the iron protoporphyrin synthesized mostly in the bone marrow (85%) and liver because of the requirements for incorporation into hemoglobin and the cytochromes, respectively. The initial and last three enzymatic steps are catalyzed by enzymes that are present in mitochondria whereas the intermediate steps are taking place in the cytoplasm.
Steps of heme synthesis
Synthesis of δ-aminolevulinic acid (ALA): In the mitochondria by ALA synthase enzyme, succinyl COA condenses with glycine to form α-amino-β-ketoadipic acid in presence of vitamin B6 which activate glycine. By the same enzyme α-amino-β-ketoadipic, acid is decarboxylated to form δ-aminolevulinic acid (ALA).
Synthesis of porphobilinogen (PBG): In the cytoplasm, 2 molecules of ALA dehydratase enzyme to form porphobilinogen (PBG) ALA dehydratase is zinc-containing enzyme inhibited by lead.
Synthesis of uroporphyrinogen: In the cytosol, four molecules of porphobilinogen condense together by uroporphyrinogen I synthase to form an open-chain tetrapyrrole which can spontaneously form uroporphyrinogen I, the linear tetrapyrrole in presence of uroporphyrinogen III cosynthase produces the asymmetrical isomer uroporphyrinogen III.
Synthesis of coproporphyrinogen: In the cytosol, all acetate groups (A) are decarboxylated to methyl substituents.
Synthesis of protoporphyrinogen III, protoporphyrin and heme: In mitochondrial coproporphyrinogen oxidase which acts only on type III oxidizes and decarboxylates two propionic side chains in rings I and II to vinyl groups (-CH=CH2) and protoporphyrinogen III is formed. Protoporphyrinogen (4 methylene bridges -CH2-), by oxidase forms protoporphyrin (4 methenyl bridges -CH=), and then by heme synthase ferrochelatase) heme is formed.
Regulation of heme synthesis
- ALA synthase enzyme controls the rate-limiting step of Heme synthesis. Heme and also hematin act as a repressor of the synthesis of ALA synthase and act as a feed-back inhibitor at this step, the inhibition occurs at an allosteric site.
- The block in heme biosynthesis in pantothenic acid or vitamin B6 deficiency occurs at a very early step in heme synthesis (ALA synthase).
- ALA dehydratase is a sulfhydryl enzyme and is very sensitive to inhibition by heavy metals as mercury or lead.
Disorder of heme biosynthesis (porphyrias)
They are a group of disorders due to abnormalities in the pathway of biosynthesis of heme, they can be genetic or acquired. Also, porphyrias can be classified according to organs or cells that are most affected into hepatic and erythropoietic on both.
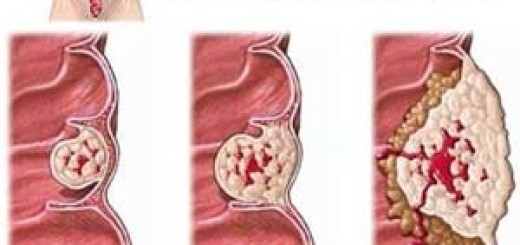
The clinical signs and symptoms of porphyria result from either deficiency of metabolic products beyond the enzymatic block of Hb biosynthesis or from an accumulation of metabolites before the block. Where the enzyme lesion occurs early in the pathway prior to the formation of porphyrinogens, ALA and PBG will accumulate in the body causing toxic effects in abdominal nerves and in CNS, resulting in abdominal pain and neuropsychiatric symptoms.
On the other hand, enzyme blocks later in the pathway result in the accumulation of porphyrinogens (colourless), which upon oxidation produces the corresponding porphyrins (coloured) that cause photosensitivity.
Types of porphyrias
- Congenital porphyrias
- Acquired (toxic) porphyrias. Caused by exposure to toxic compounds as hexachlorobenzene and heavy metals as lead which inhibits ferrochelatase and ALA dehydratase. Patients suffer from severe anemia with the accumulation of ALA and coproporphyrin III in the urine.
Treatment of porphyrias
- Avoid exposure to sunlight.
- Injection of hemin.
- Antioxidants and β-carotene.
Fate of RBs and Catabolism of Hemoglobin
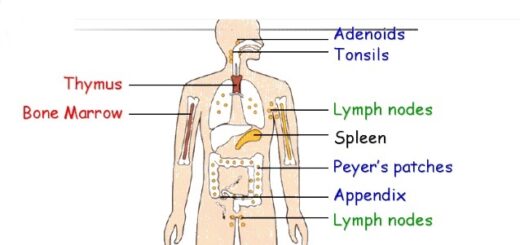
The red blood cells regularly exit from arterioles in the splenic pulp and travel through small pores to enter the splenic sinus where old red blood cells are sorted out and destroyed. Macrophages in spleen, liver, bone, marrow, etc, engulf and break down the cell fragments.
Hemoglobin is released from the cells and split into globin and heme. The globin portion is hydrolyzed into amino acids, which are reutilized for protein synthesis. The heme is converted to biliverdin and bilirubin (bile pigments, normally ∼ 0.2-0.8 mg /dL blood) that are excreted in the bile while the iron is reutilized for hemoglobin synthesis.
Blood constituents & Physical properties, Sources & functions of plasma proteins
Red blood cells (Erythrocytes) structure & function, Myeloid tissue & Bone marrow
Erythropoiesis, Hemopoiesis, Hemoglobin & Roles of red cells in oxygen transport
Hemoglobin structure, review & Types of normal hemoglobin
Abnormal types of hemoglobin, Sickling of RBCs, Types & causes of methemoglobinemia
Factors that help iron absorption, Daily iron requirements & Abnormal iron levels