Gluconeogenesis steps, regulation, importance and Maintenance of blood glucose
Synthesis of glucose (and/or glycogen) from non-carbohydrate precursors such as lactate, glucogenic amino acids, glycerol, and propionate. Liver glycogen can meet these needs for only 10-18 hours in the absence of dietary intake of CHO. During prolonged fasting, hepatic glycogen stores are depleted and glucose is formed from, non-carbohydrate precursors.
Gluconeogenesis
The major site of gluconeogenesis is the liver (90%): It can also occur in the cortex of the kidney (10%). It occurs mainly in the cytoplasm and partly in the mitochondria. It is nearly the reversal of glycolysis except for the three irreversible kinases.
The dicarboxylic acid shuttle is a mechanism by which phosphoenol-pyruvate is formed from pyruvate by the way of oxaloacetate (dicarboxylic acid). Pyruvate is carboxylated to oxaloacetate by pyruvate carboxylase. This enzyme is a liver and kidney mitochondrial enzyme but not present in the muscle.
Oxaloacetate formed is transported across the mitochondrial membrane in the form of malate. Malate is reoxidized to oxaloacetate by a NAD-linked malate dehydrogenase in the cytosol. Oxaloacetate is decarboxylated and phosphorylated to yield phosphoenol-pyruvate. This reaction is catalyzed by phosphoenolpyruvate carboxykinase (PEPCK) in the cytosol. (rate-limiting step).
Conversion of PEP to glucose
Two molecules of PEP are utilized by the reversal of glycolysis to form fructose 1,6-bisphosphate. The latter is converted to F-6-P by fructose 1,6 bisphosphate, present in liver and kidney then to G-6-P by phosphohexose isomerase. Free glucose is formed by the action of glucose 6-phosphatase in the liver and kidney, while it is absent in muscles and adipose tissues, thus glucose cannot be formed by these organs. In muscles, G-6-P can be converted to G-1-P then, to glycogen.
The gluconeogenic substrates
- Lactate: 6 high energy phosphate bonds are spent during the synthesis of glucose from 2 molecules of pyruvate.
- Glucogenic amino acids: All amino acids can give glucose except leucine (pure ketogenic). After 18 hours of fasting, proteins are considered as one of the main sources of glucose.
- Glycerol is mobilized from adipose tissues. Two molecules of glycerol are utilized for the production of one molecule of glucose in the liver and kidney in fasting or low CHO diet. Glycerol can not be utilized in adipose tissue which lacks glycerol kinase.
Importance of gluconeogenesis
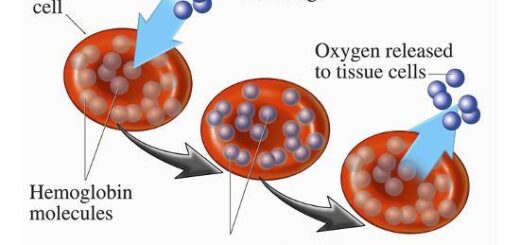
- Maintenance of blood glucose: When carbohydrates are not available in sufficient amounts e.g. starvation, prolonged exercise, and low carbohydrate diet, as glucose is an energy source to Brain tissues (the brain cannot metabolize fatty acids). glucose is an energy source for Renal medulla, testis, and faetus. glucose is an energy source for muscle and RBCs during anaerobic oxidation.
- Removal of glycerol produced by lipolysis in adipose tissues.
- Removal of lactic acid of anaerobic oxidation in RBCs and contracting muscle, thus control acid-base balance and prevent metabolic acidosis.
Regulation of gluconeogenesis
Glycolysis and gluconeogenesis are reciprocally controlled.
Long-term
Insulin is a repressor for the synthesis of gluconeogenic 4 key enzymes, and at the same time, it acts as an inducer of glycolytic key enzymes. So it inhibits gluconeogenesis.
Anti-insulin (glucagon, adrenaline, and cortisol): are secreted during fasting, stress, and severe muscular exercise. They act as inducers for these enzymes.
Short-term
- High levels of ATP & citrate allosterically stimulate F1,6 bisphosphatase.
- Excess acetyl CoA allosterically stimulates pyruvate carboxylase.
Uronic acid pathway
It is an alternative oxidative pathway for glucose that does not lead to the generation of ATP, its site is in the Liver cytoplasm, mainly. UDP glucuronic acid (the active form) is needed in:
- Conjugation to less polar compounds as bilirubin, steroids, and some drugs making them more H2O soluble (detoxicated).
- Synthesis of glycosaminoglycans (mucopolysaccharides) as heparin, hyaluronic acid,…..etc.
Citric acid cycle importance, definition, steps, products, location & inhibitors
Carbohydrate Metabolism, Importance & Hormonal regulation of glycolysis
Cellular respiration, Structure of ATP and types of fermentation
Functions of Lymphatic system, Structure of Lymph nodes, Spleen & Tonsils
Lymphatic system structure, Function of Thymus, Vascular supply & blood-thymus barrier
Immune system structure, function, cells & Types of body defense mechanisms