Citric acid cycle importance, definition, steps, products, location and inhibitors
The citric acid cycle is a part of cellular respiration, the process where your body harvests energy from the food you eat, CAC is chemical reactions used by all aerobic organisms to release stored energy through the oxidation of acetyl-CoA derived from carbohydrates, fats & proteins, into adenosine triphosphate (ATP) and carbon dioxide, The citric acid cycle offers precursors of certain amino acids, as well as the reducing agent NADH, that is used in numerous other reactions.
Citric acid cycle (CAC)
It is a series of reactions in mitochondria that brings about the catabolism of acetyl residues, liberating hydrogen equivalents which upon oxidation, leads to the release of energy. It is known as the TCA cycle (tricarboxylic acid cycle) or the Krebs cycle.
Site and steps
CAC occurs only in cells containing mitochondria. Succinyl CoA is formed by oxidative decarboxylation of α-ketoglutarate. This reaction is catalyzed by α-ketoglutarate dehydrogenase complex, consisting of three enzymes and needs 5 Coenzymes (NAD+, Coenzyme-A, FAD, lipoic acid, and TPP).
The succinyl CoA has an energy-rich bond. The cleavage of the thioester bond of succinyl CoA is coupled to the phosphorylation of guanosine diphosphate (GDP) leading to the formation of succinate and GTP. This reversible reaction is catalyzed by the thiokinase enzyme (succinyl CoA synthetase). It is the only step in CAC that yields a high energy phosphate bond directly. The γ-phosphate group of GTP is readily transferred to adenosine diphosphate (ADP) to form ATP in a reaction catalyzed by nucleoside diphosphokinase (GTP + ADP⇔ GDP + ATP).
Importance of CAC
Energy production:
Every one mole of acetyl-CoA produces 12 moles of ATP as follows:
3 NADH, H+→ 9ATP (ETC)
FADH2 → 2ATP (ETC)
ADP + Pi → ATP (Substrate level)
Total = 12 ATP
It is the amphibolic pathway i.e. both catabolic and anabolic, Catabolic functions: are the final common metabolic pathway for oxidation of carbohydrates, fats, and proteins, as they all supply acetyl CoA. Anabolic functions: The most important anabolic functions are:
- Synthesis of fatty acids and cholesterol: Citrate in high concentration is transported to the cytosol and cleaved by ATP-citarte lyase giving acetyl CoA which is used for the synthesis of fatty acid and cholesterol.
- Synthesis of non-essential amino acids: By transamination, α-ketoglutarate is converted to glutamate and oxaloacetate is converted to aspartate.
- Oxaloacetate in the cytosol is converted to PEP which is converted to glucose (gluconeogenesis).
- Heme synthesis: By providing succinyl CoA.
- Malate gives pyruvate by a malic enzyme in the cytosol, this reaction provides NADPH needed for fatty acid and cholesterol synthesis. Malate → Pyruvate + CO2
- CO2 produced is used in many important reactions including different CO2 fixation reactions, purines, and pyrimidines and urea synthesis and synthesis of H2CO3/BHCO3 buffer system.
Regulation of CAC
Short-term regulation through:
- Citrate synthase is activated by high concentrations of acetyl CoA and oxalacetate. CAC is inhibited by high concentrations of citrate and succinyl CoA.
- α-ketoglutarate dehydrogenase is inhibited by a high concentration of succinyl CoA.
- High NADH+/NAD+ and ATP/ADP ratios are inhibitors of citrate synthase, isocitrate dehydrogenase, and α-ketoglutarate dehydrogenase, while increased ADP stimulates the three enzymes.
N.B. Unlike pyruvate dehydrogenase, α-ketoglutarate dehydrogenase is not regulated by covalent modification.
Inhibitors of CAC
- Fluoroacetyl CoA combines with OAA giving rise to fluorocitrate, which inhibits aconitase enzyme.
- Malonic acid inhibits succinic acid dehydrogenase (competitive inhibition).
- Arsenite and mercury inhibit pyruvate dehydrogenase and α-ketoglutarate dehydrogenase complex by reacting with sulphhydral group of lipoic acid, leading to accumulation of pyruvic, lactic, and α-ketoglutaric acids with acidosis.
Total ATP produced from the complete oxidation of one molecule of glucose during glycolysis, oxidative decarboxylation, and CAC:
Glycolysis: G → 2PA + 8 ATP
Oxidative decarboxylation: 2PA→ 2acytyl CoA + 6 ATP (2NADH + H+×3)
CAC: 2 acetyl CoA (12 ATP ×2)
Net → 38 ATP
Pentose phosphate pathway
Hexose Monophosphate pathway (HMP) = Pentose phosphate pathway (PPP) = phosphogluconate oxidative pathway= direct oxidation of glucose
It is an alternative route for the oxidation of glucose without direct consumption or generation of ATP. It is active in the cytosol of many cells e.g. liver, adipose tissue, RBCs, adrenal cortex, ovaries, testis, retina, and lactating mammary gland. The pentose phosphate pathway occurs in two phases, oxidative and non-oxidative.
- The oxidative phase is irreversible, glucose-6-phosphate is converted to ribulose-5-phosphate with the production of two molecules of NADPH.
- The non-oxidative phase is reversible. It ends with fructose-6-phosphate and glyceraldehyde-3-P.
Importance of HMP
- HMP is the only way of R-5-P production in our body, which is needed for nucleosides, nucleotides, nucleic acids, and coenzymes biosynthesis.
- It is the main generator of reduced Coenzyme II (NADPH+H+) which is needed in reductive biosynthesis.
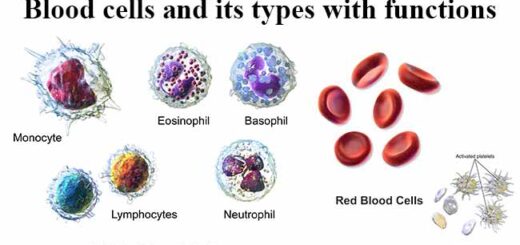
- Importance of HMP in Red cells: Red cells are liable for oxidative damage by H2O2 due to their role in O2 transport. In RBCs, H2O2 causes both oxidations of iron in hemoglobin to form methemoglobin and lipid peroxidation. Lipid peroxidation increases the cell membrane fragility.
The major role of HMP in red cells is the production of NADPH, which protects these cells from oxidative damage by providing reduced glutathione for removal of H2O2.
Regulation of the pentose phosphate pathway
The reaction catalyzed by G6P dehydrogenase is the rate-limiting in the oxidative branch i.e. the control site. The most important regulatory factor is the level of NADP+. NADPH accumulation produces feedback inhibition of glucose-6-phosphate dehydrogenase.
The flow of G-6-P in PPP depends on the need for NADPH+H+, R-5-P, and ATP. Synthesis of G6PD is induced during feeding and repressed during fasting. Insulin, which is secreted in response to hyperglycemia, increases the rate of glucose oxidation by HMP. Insulin induces the synthesis of G6PD and 6-phosphogluconate dehydrogenase.
Carbohydrate Metabolism, Importance & Hormonal regulation of glycolysis
Cellular respiration, Structure of ATP and types of fermentation
Functions of Lymphatic system, Structure of Lymph nodes, Spleen & Tonsils
Lymphatic system structure, Function of Thymus, Vascular supply & blood-thymus barrier
Immune system structure, function, cells & Types of body defense mechanisms
Gluconeogenesis steps, regulation, importance & Maintenance of blood glucose