Antimicrobial drugs types, use, side effects, resistance and Empiric antimicrobial therapy
Antimicrobial drugs are used for the treatment, control, and prevention of bacterial diseases, they are used for growth promotion and improvement of feed efficiency in the agri-food industry, Some of them are essential for the treatment of serious life-threatening infections in humans, it is imperative to develop measures to limit the development of antimicrobial resistance and to mitigate the loss of effectiveness of these life-saving drugs.
Antimicrobial drugs
Antimicrobial drugs are groups of synthetic, semisynthetic, or naturally occurring chemicals that selectively inhibit specific organisms causing infectious diseases. Antimicrobial drugs are intended to eliminate foreign organisms from the healthy tissues of the patient without effects on the normal tissue cells of the host.
This essential property of these drugs is called selective toxicity, which is relative, rather than absolute, requiring that the concentration of the drug be carefully controlled to attack the microorganisms while still being tolerated by the host.
According to the spectrum of antimicrobial activity, antimicrobial drugs include the following:
- Antibacterial drugs.
- Drugs Used in Tuberculosis.
- Antiviral Drugs.
- Antifungal Drugs.
- Antiprotozoal Drugs.
- Anthelminthic Drugs.
In the following chapters, the indicated topics will be covered:
- General Principles of Antimicrobial Therapy.
- Antibacterial Drugs.
- Antifungal Drugs.
- Anti-herpetic Drugs.
- Anthelminthic Drugs.
General Principles of Antimicrobial Therapy
General principles of antimicrobial drugs prescription
General principles when prescribing antimicrobial therapy should be followed to benefit both the individual patient and the community. These include:
- Diagnosis.
- Cause of infection; bacterial, viral, or others.
- The goal of the therapy i.e empirical, prophylaxis, or definitive treatment of an infection.
- Antimicrobial selection.
- Good knowledge of the drug’s pharmacokinetics, pharmacodynamics, and potential risk.
- Appropriate antimicrobial drug dosage.
- A suitable length of the treatment period.
- Antimicrobial combinations should be used only under certain conditions and the right choice of combinations.
The goal of antimicrobial therapy
The goal of antimicrobial therapy is either one of the following:
- Empiric therapy: used for initial control of infection when the organism is not yet identified.
- Prophylaxis: to prevent infection, e.g, antibiotic prophylaxis to prevent postoperative surgical wound infection.
- Definitive therapy: used definitely to cure the infection of a known etiology and antimicrobial susceptibility.
Empiric antimicrobial therapy
Although the microbiological diagnosis is ideally based on data such as bacterial or fungal culture or serologic testing, frequently the most likely microbiological etiology can be inferred from the clinical presentation. When a patient does not benefit from empiric antimicrobial therapy, additional investigations are needed to determine the etiologic agent or exclude noninfectious diagnoses.
The guessing of the pathogen for antimicrobial empirical treatment choice depends on the following:
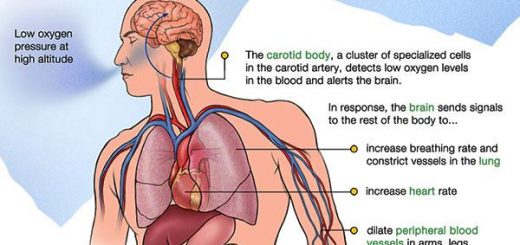
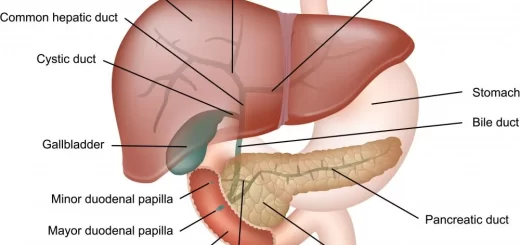
1. Anatomic site of infection, i.e., respiratory tract, urinary tract, skin and soft tissue, gastrointestinal tract, genital tract, etc. each has its typical list of micro-organisms. In respiratory tract infections, empirical antibiotic treatment should cover Streptococcus pneumoniae, in the skin and soft tissue infections, empirical treatment should target Staphylococcus aureus and Streptococcus pyogenes, while in urinary tract infections, the therapy should be effective against Escherichia coli.
2. Age, especially its extremes, may change the spectrum of pathogens in some infections. In bacterial meningitis, Listeria monocytogenes plays a greater role in neonates and patients above 50 years of age.
3. Resistant bacteria are more common in hospitals and in nursing homes than in community-acquired infections.
4. History of travelling to countries, which are endemic in some diseases, as well as pattern of microbial resistance in these regions, e.g., chloroquine resistant malaria in Thailand.
5. History of recent antibiotic exposure in the recent past (approximately 3 months) can also help in selection of antimicrobial therapy. Because the causative microorganism for a current episode of infection is likely to be resistant to that drug and/or drug class, and an alternative agent should be used.
6. In seriously ill hospitalized patient, because microbiological results do not become available for 24 to 72 hours, initial therapy for infection is often empiric and guided by the clinical presentation. Therefore, a common approach is to use broad-spectrum antimicrobial agents or sometimes a combination of antimicrobial agents with the intent to cover multiple possible pathogens.
Once microbiology results have helped to identify the etiologic pathogen and/or antimicrobial susceptibility data are available, every attempt should be made to narrow the antibiotic spectrum, This is a critically important component of antibiotic therapy because it can reduce cost and toxicity and prevent the emergence of antimicrobial resistance in the community.
You can follow science online on Youtube from this link: Science online
You can download Science online application on google Play from this link: Science online Apps on Google Play
Parasitic infections, Immunological tests, DNA probes and Polymerase Chain Reaction
Diagnosis of parasitic infections and Techniques used for identification of Intestinal Parasites
Myiasis classification, diagnosis, causes, treatment & medicolegal importance
Importance & types of fungi, Opportunistic infections & Predisposing factors to candidosis
Vaccines types, Live vaccines, Inactivated vaccines, Subunit vaccines, Naked DNA & mRNA vaccines
Features and classification of viruses, Defective viruses and Viral vectors used for gene therapy