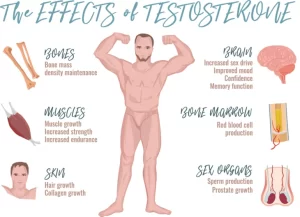
Testosterone effects, low testosterone symptoms, Hypogonadism and Hypergonadism in male
Testosterone is a steroid formed by the interstitial cells of Leydig. Leydig cells are almost non-existent in the testes during childhood, but they are numerous in the newborn male infant and also in the adult male after puberty, at both these times the testes secrete large quantities of testosterone.
Testosterone hormone
Testosterone is transported in the plasma bounded to proteins; albumin and β globulin. Like steroid hormone, testosterone binds to cytoplasmic receptors in the target cells and increases the transcription of mRNAs which stimulate protein synthesis and alter cell functions. A small amount of testosterone is converted into estrogen. However, most testosterone is converted into 17-kctosteroids which are excreted in the urine.
Functions of testosterone during fetal development
Male chromosome causes the newly developing genital ridge to differentiate into cells that secrete testosterone while the female chromosome causes this ridge to secrete estrogens. Testosterone is responsible for:
- The development of the male sex organ including the formation of the penis, scrotum, prostate gland, seminal vesicles, and male genital ducts.
- Suppressing the formation of female genital organs.
- Descending of the testis into the scrotum during the last 2-3 months of pregnancy.
- Effect of testosterone on the development of adult primary and secondary sexual characteristics.
Functions of testosterone at puberty
Testosterone is responsible for the initiation and maintenance of body changes associated with puberty in man.
- On external genitalia: it causes enlargement of the penis, the scrotum, and the testes
- On internal genitalia: it causes enlargement of the seminal vesicle, the prostate and bulbo-urethral gland.
- On secondary sexual characteristics:
Hair growth: the body hair increases particularly in the face (so the beard and moustache appears), chest, limbs axillae, and around the anus The pubic hair grows in the form of a triangle with its apex up However, the scalp hair falls with the bilateral temporal recession of the frontal scalp hairline, and boldness is accelerated.
Voice changes: it causes hypertrophy of the laryngeal mucosa and enlargement of the larynx. The vocal cords increase in length and thickness so the voice becomes deeper.
Skin changes: it increases the thickness of the skin over the entire body and increases the ruggedness of the subcutaneous tissues. It increases the rate of secretion of sebaceous glands (over-secretion of these can result in acne).
Psychological changes at puberty, boys become aggressive and their interest in sex develops with increased libido (sexual desire).
Changes in the body conformation: the shoulders broaden and the muscles enlarge due to the anabolic effect of testosterone.
Testosterone increases protein formation and muscle development: anabolic functions. It increases musculature following puberty and increases protein in other parts of the body as well. Many of the changes in the skin are due to the deposition of proteins in the skin. This anabolic effect will lead to:
- Testosterone can increase the basal metabolic rate by 15%.
- It stimulates the secretion of erythropoietin and increases the number of red blood cells.
- It can increase the reabsorption of sodium in the kidneys, thus it can increase the blood and extracellular fluid volumes of the male.
Effect on bone
- It increases the total quantity of the bone matrix and it also causes calcium retention due to its anabolic effect.
- Lengthening of the pelvis with narrowing of its outlet. The pelvis becomes funnel-like shape instead of the broad ovoid shape of the female pelvis. This increases the strength of the entire pelvis for load-bearing.
- It also causes the epiphyses of the long bones to unite with the shafts at an early age.
Testosterone has important effects on lipid metabolism. It increases circulating low-density cholesterol and decreases circulating high-density cholesterol and favors accumulation of upper body abdominal and visceral fat.
Control of Male Sexual Functions
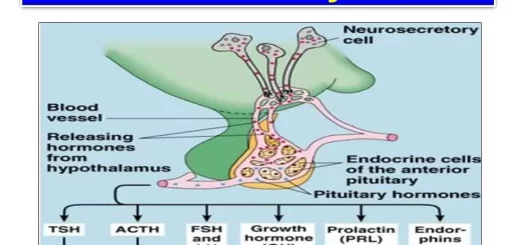
1. Hypothalamic regulation:
Near the age of puberty, the cell bodies of neurons of arcuate nuclei of the hypothalamus begin to secrete gonadotropin-releasing hormone (GnRH), widely known as LH-releasing hormone into the hypothalamic-hypophysial portal vascular system. This hormone in turn stimulates the anterior pituitary gland to secrete gonadotropic hormones: luteinizing hormone (LH) and follicle-stimulating hormone (FSH). In turn, LH is the primary stimulus for the secretion of testosterone by the testes, and FSH mainly stimulates spermatogenesis.
2. Anterior Pituitary regulation:
The anterior pituitary gland secretes gonadotrophic hormones: FSH & LH hormone luteinizing hormone (LH). These are glycoprotein hormones. In adult, luteinizing hormone, in turn, stimulates hyperplasia of the Leydig cells of the testes and also stimulates the production of testosterone by these cells and FSH stimulates spermatogenesis.
During pregnancy, the placenta secretes large quantities of human chorionic gonadotropin, a hormone that has almost the same properties as LH. This hormone stimulates the formation of Leydig cells in the testes of the fetus and causes testosterone secretion
3. Feedback control of testosterone secretion:
The secreted testosterone feeds back negatively to the hypothalamus inhibiting the production of GnRH that in tum decreases LH and FSH secretion from the anterior pituitary.
4. Feedback control of spermatogenesis: Spermatogenesis by the testes inhibits the pituitary secretion of FSH. Sertoli cells are probably responsible for most of the feedback control of FSH secretion and of spermatogenesis. These cells secrete inhibin that has a direct inhibitory effect mainly on the anterior pituitary gland to inhibit the secretion of FSH.
Puberty and regulation of its onset
During childhood, the hypothalamus does not secrete a significant amount of gonadotropin-releasing hormone and consequently, almost no testosterone is secreted. This may be due to that the slightest secretion of sex steroid hormones exerts a strong inhibitory effect on hypothalamic secretion. Yet, for reasons still not understood, at the time of puberty, the secretion of hypothalamic GnRH breaks through childhood inhibition and adult sexual life begins.
Hypogonadism in male
It means decrease secretion of male sex hormones. Hypogonadism is caused by:
- The person may be born without functional testes.
- He may have undeveloped testes.
- Cryptorchidism (undescended testes).
- He may lose his testes which is called castration.
- A rare child is born who has a genetic absence of androgen receptors in the target cells. In such a child, testosterone is often formed in abundance, but still it has no masculinizing effect.
Characters of hypogonadism
When a boy loses his testes before puberty:
- He will have infantile sexual characteristics throughout life.
- Sexual organs and secondary sexual characteristics are those of a child.
- The voice is childlike
- There is no loss of hair on the head, and normal masculine hair distribution on the face and elsewhere does not occur
- The height is slightly greater than that of the normal man, though the bones are quite thin.
- The muscles are weaker than those of normal.
When a man is castrated following puberty:
- Some male secondary sexual characteristics revert to those of a child and others remain of masculine character.
- Sexual organs regress slightly in size.
- Voice regresses from the bass quality only slightly.
- There is loss of masculine hair distribution.
- Loss of the thick masculine bones.
- Loss of the musculature of the virile male.
Hypergonadism in male
It occurs if there is a tumor in the interstitial Leydig cell. It secretes large quantities of testosterone. When such tumors develop in young children, they cause:
- Rapid growth of the musculature and bones but also early union of the epiphyses so that the height of the adult is actually less than the normal subject.
- It causes excessive development of the sexual organs and of secondary sexual characteristics.
You can download Science online application on Google Play from this link: Science online Apps on Google Play
Organs of male genital system, Structure of the testis, Functions of Sertoli cells & Leydig cells
Testis functions, sperms production, Factors affecting spermatogenesis, Structure of Epididymis
Vas deferens function, histology, anatomy, Varicocele & Functions of Seminal vesicle
Prostate function, structure, lobes, Benign enlargement of prostate & malignant prostatic tumor