Physiology of pain sensation, Types of pain receptors, Effects of somatic pain and Visceral pain
Pain is an unpleasant sensory and emotional experience associated with actual or potential tissue damage, The person’s estimate of the magnitude of a painful stimulus depends very much on his personality and emotional state at the time; therefore it is not easily evaluated and an objective technique for measuring pain is unreliable.
Physiology of pain sensation
Pain receptors (Nociceptors) are sensory receptors that detect signals from damaged tissue, The impulses from the nociceptors are transmitted via two fiber types, thinly myelinated Aδ and unmyelinated C fibers.
Types of pain receptors
- Mechanosensitive pain receptors: stimulated by intensive pressure applied to the skin.
- Thermosensitive pain receptors: stimulated by extremes of temperature. These are cold-pain receptors (stimulated by temperature between 0 and 10 °C) and hot pain receptors (stimulated by temperature above 45 °C).
- Chemically sensitive pain receptors: respond to various chemicals like bradykinin, histamine, high acidity, serotonin, proteolytic enzymes, lactic acid, prostaglandins, and environmental irritants.
- Polymodal pain receptors: stimulated by high-intensity mechanical, thermal (hot and cold) or chemical stimuli.
Types of pain
It can be classified into:
A. Nociceptive pain: include;
- Somatic pain, could be cutaneous or deep.
- Visceral pain.
B. Neuropathic pain: due to disease of peripheral, cranial nerve or CNS.
I. The somatic pain
Somatic pain can be cutaneous if produced by stimulation of pain receptors in the skin and subcutaneous tissues; or deep if produced by stimulation of pain receptors in muscles, ligaments, tendons, and periosteum of bones. Deep pain is poorly localized, dull aching, and commonly associated with autonomic parasympathetic effects such as bradycardia, hypotension, nausea, and vomiting.
Cutaneous pain
Cutaneous pain is conducted from pain receptors through two types of afferent fibers giving double pain sensation, a fast pricking immediate pain, and a slow-burning or dull aching delayed pain.
- Fast pain is cutaneous pain of short duration, transmitted along rapidly-conducting thin myelinated A-δ fibers, (2-5 μm in diameter) that conduct at rates of ∼12-35 m/s, It is of short duration, well-localized, transmitted by the spinothalamic (neospinothalamic) tract.
- Slow pain can be cutaneous or deep transmitted by the slowly conducting unmyelinated C fibers, (0.4-1.2 μm in diameter) that conduct at low rates of ∼ 0.5-2 m/s, It lasts for a long duration, dull and diffuse (poorly localized), transmitted by the spinoreticular (paleospinothalamic) pathway.
Reactions (effects) of somatic pain
- Somatic reflexes: fast pain initiates the withdrawal reflex which takes the body away from the noxious stimulus.
- Autonomic effects: cutaneous pain is usually associated with sympathetic effects (e.g. V.C., tachycardia, and rise of arterial B.P.) but if severe parasympathetic effects may occur (e.g.V.D., bradycardia, and hypotension).
- Emotional effects: (e.g. crying, restlessness, and anxiety) due to the stimulation of the limbic system.
- Cutaneous hyperalgesia (tenderness): hyperalgesia is a condition of increased sensitivity to pain that often accompanies various inflammatory conditions of the skin.
There are 2 types of cutaneous hyperalgesia:
1. Primary hyperalgesia
Occurs in the area of red skin i.e. area of flare that surrounds an inflammed or injured skin area. In this area, the threshold of pain receptors is lowered so that weak non-painful stimuli e.g. touch produce pain.
Mechanism: Primary hyperalgesia is caused by the diffusion of pain-producing substances e.g. histamine, proteolytic enzymes, and kinins from the injured skin area to neighboring healthy skin resulting in vasodilatation (redness) and lowering the threshold of pain receptors in this area.
2. Secondary hyperalgesia
Secondary hyperalgesia occurs in the healthy skin area beyond the area of flare, In this area, the pain threshold is not lowered, but painful stimuli cause an increased central effect ie, the pain sensation produced is more severe and prolonged than normal.
Mechanism: There is increased excitability of the dorsal horn cells following tissue injury this increased excitability is called central sensitization Since afferent fibers from both the area of skin injury and the area of secondary hyperalgesia converge on the same dorsal horn neurons.
Therefore usual painful stimuli applied to the area of secondary hyperalgesia, produce an exaggerated pain sensation than excepted, Central sensitization is an increase in the excitability of neurons within the CNS, so that neural input produces an abnormal response.
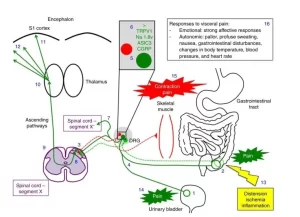
II. The visceral pain
The viscera contain relatively few pain receptors and pain impulses are conducted from them by slow-conducting C-fibers (true visceral pain). Some viscera e.g. the lung’s alveoli, liver parenchyma, and the brain are insensitive to pain because they contain no pain receptors. On the other hand, the parietal layers of the pleura, peritoneum, and pericardium are richly supplied with pain receptors, impulses from these membranes are transmitted by Aδ fibers (parietal visceral pain).
Characters of visceral pain
True visceral pain (resulting from stimulation of pain receptors in the viscera itself, is dull aching, and poorly localized. Whereas parietal pain (resulting from stimulation of pain receptors in the parietal coverings) is mostly sharp, severe, and better localized.
Visceral pain is commonly associated with autonomic parasympathetic effects such as bradycardia, hypotension, nausea, and vomiting. It may be associated with reflex contraction of muscles of the anterior abdominal wall, which helps to protect the underlying visceral structures. It is often referred to other areas (referred pain).
Afferents for visceral pain
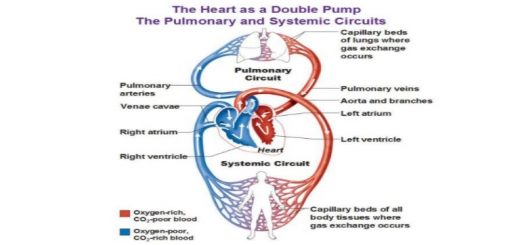
True visceral pain is transmitted through autonomic visceral afferents. Afferent fibers from visceral structures reach the CNS via nerve fibers that travel with sympathetic and parasympathetic nerves, Their cell bodies are located in the dorsal root ganglia and the homologous cranial nerve ganglia.
Specifically, there are visceral afferents in the facial, glossopharyngeal, and vagus nerves; in the thoracic and upper lumbar dorsal roots; and in the sacral dorsal roots, On the other hand, parietal visceral pain is transmitted by somatic afferent e.g. the phrenic and thoracic intercostal nerves transmit pain sensation from the parietal pleura, pericardium and peritoneum.
Causes of visceral pain
- Spasmodic contraction of hollow viscera as the uterus or intestine as well as overdistension e.g. urinary bladder overfilling, both conditions result in ischemic pain due to compression of blood supply.
- Thrombosis of blood vessels supplying the viscus results in ischemic pain as in the case of coronary thrombosis, Insufficient blood supply to the viscus results in the accumulation of metabolites such as lactic acid or produces tissue damage which releases pain-producing substances.
- Visceral inflammatory processes and ulcerations as gastric ulcers result in chemical irritation and pain.
You can subscribe to science online on YouTube from this link: Science Online
You can download Science Online application on Google Play from this link: Science Online Apps on Google Play
Referred pain examples, Causes of neuropathic pain & Pain control mechanisms
Ascending tracts for somatic sensations and Deficits after lesions in the dorsal column pathway
Physiology of sensory receptors, Coding of sensory information & Somatic sensation
Function of sensory nervous system, Histological structure of ganglia and receptors
Cranial nerves types, Facial, Vestibulocochlear, Glossopharyngeal, Vagus, Accessory & Hypoglossal
Skull function, anatomy, structure, views & Criteria of neonatal skull