Mechanics of Pulmonary Ventilation and Pressure changes during Respiratory cycle
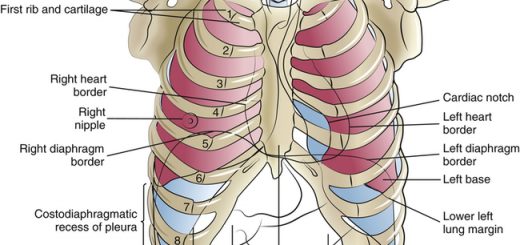
The lungs can be expanded & contracted in two ways; By downward and upward movement of the diaphragm to lengthen or shorten. By elevation and depression of the ribs to increase and decrease the transverse and anteroposterior diameters of the chest cavity.
Mechanics of Pulmonary Ventilation
In normal quiet breathing, inspiration is an active process due to the contraction of inspiratory muscles, but expiration is a passive process.
Mechanics of Inspiration:
Normal resting inspiration is brought about by contraction of the main muscles of inspiration as:
- The Diaphragm: When it contracts, the abdominal contents are forced downward and forward and the vertical dimension of the chest cavity is increased, In addition, the lower rib margins are lifted and moved out, causing an increase in the transverse diameter of the thorax.
- The external intercostal muscles: When they contract, the ribs are pulled upward like a bucket handle (increasing the transverse diameter of the thorax), and outward pushing the sternum upward and forward like a pump handle (increasing the anteroposterior diameter of the thorax).
By contraction of the diaphragm and external intercostals, the chest cavity is expanded in all dimensions, leading to expansion of the lungs as well. The pressure inside the lungs falls down, and the air is drawn into the lung (inspiration).
Forced inspiration: In addition to the contraction of the diaphragm and external intercostal muscles, other accessory muscles of inspiration come into action as:
- Scalene muscles which elevate the first two ribs.
- Sternomastoid muscles which raise the sternum.
- Serratus anterior muscles which lift many of the ribs.
Mechanics of Expiration
Normal quiet expiration is passive. During expiration, the inspiratory muscles simply relax. The elastic recoil of the lungs, chest wall, and abdominal structures, as well as the drop of the thoracic cage by its weight, compress the lungs and expel the air outside. The thorax returns back to the resting expiratory level (mid-thoracic position).
Forced expiration, as during exercise or voluntary hyperventilation, is active, The elastic forces are not powerful enough to cause the necessary rapid expiration, so that extra force is achieved, mainly by contraction of the expiratory muscles. The most important muscles of expiration are:
- The abdominal wall muscles as the rectus abdominus, internal and external oblique, and transversus abdominus. When these muscles contract intraabdominal pressure is raised and the diaphragm is pushed upward thereby compressing the lungs, increasing the pressure inside, and pushing air forcefully out.
- The internal intercostals which run downward and backward contract, They pull the ribs downward and inward thus decreasing the thoracic volume.
Pressure changes during the respiratory cycle
There are three pressures responsible for the movement of air in and out of the lungs. These pressures are intrapleural pressure (IPP), intraalveolar or intrapulmonary pressure (IAP), and transpulmonary or distending pressure.
Intra-pleural pressure (IPP)
There are no attachments between the lung and the walls of the chest cage, except where it is suspended at its hilum from the mediastinum. Instead, the lung “floats” in the thoracic cavity, surrounded by a thin layer of fluid (pleural fluid) that lubricates the movement of the lungs within the cavity.
Furthermore, continual auction of excess fluid into lymphatic channels maintains a slight suction between the visceral and the parietal pleural surfaces. Therefore, the lungs slide easily on the chest wall, but resist being pulled away from it, in the same way, that two moist pieces of glass slide on each other but resist separation.
Normally, no air exists in pleural space but rupture of the lung by a penetrating wound can cause air (pneumothorax), fluid (hydrothorax), blood (haemothorax), or pus (pyothorax) to enter leading to lung collapse.
Definition of IPP
It is the pressure in the “potential space” between the lungs and chest wall (pleural space). It is a negative pressure (subatmospheric).
Causes of negativity of IPP
- Lack of air in the pleural cavity.
- Elastic recoil of the lung which continuously pulls against the continuous tendency of the relatively rigid chest wall to expand. This creates a continuous negative pressure that antagonizes the elastic recoil of the lung. The elastic recoil of the lung is due to the elastic fibers of the lung tissue which are continuously stretched and always tending to recoil. This accounts for about one-third of recoil, and due to the surface tension of the fluid lining the alveoli. This accounts for about two-thirds of recoil.
- Elastic properties of the chest wall which tend to expand the thoracic cage thus it pulls the parietal pleura outwards.
Significances of negative IPP
- It helps in the expansion of the lungs.
- It is responsible for the negative intrathoracic pressure which also helps: Venous return to the heart, and Lymphatic flow in the thoracic duct.
IPP during normal quiet breathing:
The normal pleural pressure at the beginning of inspiration is about 5 cm H₂O, which is the amount of suction that is required to hold the lungs open to their resting level. Then during normal inspiration, the expansion of the chest cage pulls the surface of the lungs with still greater force and creates a still more negative pressure down to an average of about -7.5 cm H₂O.
These relations between pleural pressure and changing lung volume are demonstrated in showing in the bottom panel the increasing negativity of the pleural pressure from -5 to -7.5 cm H₂O during inspiration and in the top panel an increase in lung volume of 0.5 liter. Then, during expiration, the events are essentially reversed.
Alveolar pressure (intrapulmonary pressure)
Alveolar pressure is the pressure of the air inside the lung alveoli, When the glottis is opened and no air is flowing into or out of the lungs, the alveolar pressure is equal to the atmospheric pressure (zero cm H₂O).
During inspiration, the increased volume of alveoli as a result of lung expansion decreases the intra-alveolar pressure to a value below atmospheric pressure of about -1 cm H₂O, This slight negative pressure is enough to move 500 ml of air into the lungs in 2 seconds required for inspiration, At the end of inspiration, the alveolar pressure returns to the atmospheric pressure (zero cm H₂O).
During expiration, opposite changes occur, The lung alveoli collapse before the air is expelled from them, The alveolar pressure rises to about +1 cm H₂O, This forces the 500 ml of inspired air out of the lung during 2-3 seconds of the expiration. By the end of expiration, the pressure drops gradually and becomes atmospheric again.
Diaphragm anatomy, structure, function, Phrenic nerves and Nerves of the thorax
Lung structure, borders, Lobes, Fissures and Broncho-pulmonary segments
Trachea, Major Bronchi, Thoracic cavity structure, function and anatomy
Larynx structure, function, cartilages, muscles, blood supply and vocal folds