Upper GI Bleeding cause, symptoms and How do you treat upper GI bleeding?
Upper gastrointestinal (GI) bleeding refers to bleeding from the esophagus, stomach, or duodenum (proximal to the ligament of Treitz). It can range from mild to life-threatening and requires prompt evaluation and management.
Upper GI Bleeding
Presentation:
1. Haematemsis: The bleeding site is no more distal to the duodenum.
Vomiting of:
Fresh blood → significant bleed.
Small amount of altered blood (coffee grounds) → small bleed that already settled.
2. Black Stool:
Detailed questioning:
- Melena: Liquid, jet black or black with a reddish tinge pungent characteristic smell quite unlike the smell of feces.
- Dark-formed stools →→ insignificant.
- Iron therapy sticky feces with dark grey rather than black.
- Bleeding from the colon rarely melaena as the blood passes too quickly for the heme to be oxidized.
- Massive bleeding may be fresh rectal bleeding.
Activity of bleeding
- Grossly bloody haematemsis or large fresh clots per rectum.
- Active bleeding → 2 to 3 fold mortality.
- NG aspirate may be negative in 10% of bleeding D.U. due to oedema or pylorospasm (failure of blood reflux into the stomach).
- The sensitivity of NG aspirate in assessing active bleeding is 79%.
Sites
1. Oesophagus Bleeding
Causes
- Varices 75%
- Oesophagitis
- Ulcers
- Neoplasm.
- Mallory Weiss tear → longitudinal tear in the mucosa.
- Hiatus hernia.
- Rarely require urgent surgery.
2. Stomach
- Gastritis.
- G. cancer.
- G. ulcer.
- G. varices.
- Rupture retro gastric aneurysm.
- A-V malformation.
3. Duodenum
- Duodenitis.
- Haemobilia.
- D.U.
- Neoplasm.
- AV malformation. (Aortoenteric fistula).
- Diverticulum.
- Crohn’s disease.
Most common causes in Egypt (in order of frequency)
- Esophageal varices (75%).
- Erosive gastritis.
- Duodenal ulcer (DU).
- Cancer stomach.
- Gastric ulcer (GU).
The severity of the attack can be evaluated by the presence and extent of hypovolemia.
- Mild: no significant hypovolemia.
- Moderate: hypovolemia that responds to volume replacement (crystalloids and blood) and thereafter the patient is stable.
- Severe: active continued major bleeding rendering resuscitation with blood transfusion difficult, or recurrent major re-bleeding after successful resuscitation.
Presentation according to onset
- Sudden massive hematemesis → shock.
- Slow (usually melena) chronic anemia.
Management:
Resuscitation
All patients should be kept nothing by mouth at least until endoscopy has been performed.
Fluid replacement and blood transfusion.
- Send blood for grouping and save, and start glow IV.
- Blood transfusion if Hgb is <10 g/dl with evidence of acute blood loss.
- Goal of a hematocrit value (HCV) > 30%.
- Rapid transfusion in hemodynamically stable patients should be avoided (Heart failure and re-bleeding).
- Warm the blood to 25oC by warmer.
- Fresh frozen plasma (FFP) every 6 units of stored blood (15 ml/kg) or every 4 U-packed RBCs.
- Citrate toxicity is avoided by 10 ml of 10% Ca gluconate after the first 6 units and then every 2 subsequent units. Hypokalemia is carefully monitored.
Surgical Treatment
Indications of Surgery
- Patients with severe hemorrhage that resuscitation with volume replacement cannot keep up with the losses.
- Elderly patients older than 60 y if> 4 units of blood are necessary during the initial resuscitation and patients who has one recurrence of bleeding after initial successful control.
Lines of Surgery
- The use of a definitive ulcer-curing operation is mandatory in patients with hemorrhage, but is optional in patients with perforation.
- Pyloromyotomy under run the vessel.
- PG or TV + GJ (truncal vagotomy and gastro-jejunostomy).
- Recurrent bleeding in both is 13%.
- Mortality of PG 8% is double that of TV + GJ.
Stable patient
- Send blood for grouping and save, start, slow I.V
- Blood transfusion if Hb is less than 10 g/dl with evidence of acute blood loss.
- Chronic anemia is better treated with blood.
- Rapid transfusion in hemodynamically stable should be avoided (HF & re-bleeding).
Massive transfusion
- The goal of a hematocrit value of over 30%.
- Fresh frozen plasma every 6 units of stored blood (15 ml/kg) or every 4 U-packed RBCs.
- Citrate toxicity is avoided by 10 ml of 10% Ca gluconate after the first 6 units and then every two subsequent units.
- Hypokalemia carefully monitored.
- Warm the blood to 25oC by warmer.
- BT is prolonged when the platelet count is below 70,000 → replacement.
Endoscopic Haemostasis (Within 24hrs)
- Injection methods adrenaline, alcohol STD, and polidocanol.
- Laser photocoagulation “Argon, Nd YAG”.
- Diathermy→ bipolar or monopolar.
- Heater probe.
Other methods
- Topical agent – Collagen, clotting factors, cyanoacrylate glue, fibrin sealant, thrombin.
- Mechanical methods – Clips, staples, sutures.
- Microwave & argon plasma coagulator (APC).
We should use more than one agent eg adrenaline + clips.
Heater probe
1. Monopolar
- No electrical current only heat, unlike diathermy.
- Heating to 100°C.
- severe tissue injury.
2. Bipolar diathermy (Multipolar)
- More concentrated energy to a very specific area of tissue.
- As treated tissues dries up→ (no sticking to the tissue.
Results: Rebleeding, mortality decreased.
Laser Photocoagulation
- Non-contact thermal device but high cost.
- Energy converted to heat coagulation→ haemostasis.
- Argon 440-520 nm wavelength.
- Nd YAG over 1000 nm wave length→ more effective, deeper penetration.
Injection treatment:
- Adrenaline (1:10,000): Tissue pressure Active vasospasm, Activation of platelet.
- Sclerosants STD, polidocanol thrombosis by damaging the endothelium.
- Absolute alcohol → rapid dehydration of tissue fixation.
With Stopping of Bleeding:
After 12-24 hrs he can eat→ good for morale.
Muscle contraction→ ↓ acidity.
Monitor:
- twice daily hematocrit.
- occult blood in stools.
Oesophageal Varices
- 75% of Upper GI Bleeding.
- Varices Bleed in the Distal 3-5 cm of the Oesophagus.
- Endoscopic Diagnosis:
A. Bleeding:
- Oesophageal varix + bright red blood.
- venous (non-pulsatile).
B. Non bleeding varices (50-70%):
White nipple sign (platelet plug on the surface of a varix).
Bleeding Varices
In 75% of patients, bleeding ceases spontaneously of them 60% will re-bleed, the risk:
- During the first 5 days.
- With severe hepatic disease.
Prognostic Factors:
- Rebleeding.
- Continued bleeding within 5 days.
- Active bleeding at endoscopy.
Management
1. Resuscitation + Vit. K: IV., maximum daily doses.
- Correct hypokalaemia and hypoglycaemia # encephalopathy.
- Enema helps get rid of NH4.
2. Medical Management
Vasopressin/ Glypressin (VC).
Vasopressin: IV bolus: 20 units/100 ml G 5%/20 min or Infusion 0.4 units/min. It has 3 side effects; myocardial infarction, gut ischemia & local gangrene.
Glypressin: It has lower side effects. Bolus dose, longer action
Somatostatin (Octerotide):
- Inhibits peptide secretion (gastrin, glucagon, CCK, VIP).
- Inhibits Gl exocrine secretion gastric, pancreatic.
- Slows Gl transit time.
- Decrease blood flow, inhibits postprandial, and increases portal hypertension.
- Synthetic analogue (Octereotide), half-life 1-2 hours, greater potency, little side effects. Dose = mg/8 h for 48 hours on 250 ml of glucose 5%.
3. Upper Gl endoscopy
Band ligation/Sclerotherapy:
Banding:
- No retrosternal pain.
- Superficial ulcers.
- G. varices.
- Equal efficacy.
- Safer.
Sclerotherapy:
- Minor chest pain, and fever.
- Chest complication.
- Oesophageal ulcer.
- Dysphagia.
- Stricture.
Propanolol (for future prophylaxis NOT during the attack).
4. Surgery
Indications (about 25%): Nonstoppage of bleeding after 2 sessions of sclerotherapy, Bleeding gastric varices (5-50% of cases).
Operative lines:
- Emergency decongestion: Mortalityol 40%. Portal vein thrombosis occurs in 30% of cases.
- The emergency porto-caval shunt is obsolete.
- The preferred technique is esophageal transection with stapling.
TIPS Transjugular intrahepatic portosystemic shunt):
- It can be done anywhere but is usually done between the Rt tributary of the portal vein and the Rt hepatic vein.
- Bypass liver (no detoxification>> HE).
- Bridge therapy
- Needs good coagulation (liver disease?!).
You can subscribe to Science Online on YouTube from this link: Science Online
You can download Science online application on Google Play from this link: Science online Apps on Google Play
Gastroesophageal Reflux Disease, Complications of GERD and Barrett’s oesophagus
Esophagus diseases, Dysphagia causes, Achalasia, and Symptomatic Diffuse Esophageal spasm
Pharynx function, anatomy, location, muscles, structure, and Esophagus parts
Tongue function, anatomy, and structure, Types of lingual papillae, and Types of cells in taste bud
Mouth Cavity divisions, anatomy, function, muscles, Contents of Soft palate and Hard palate
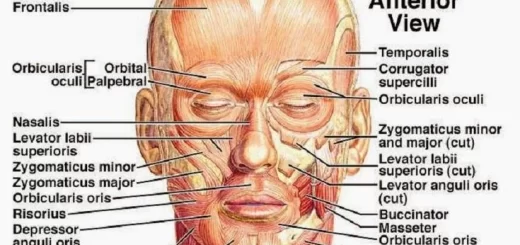
Temporal and infratemporal fossae contents, Muscles of mastication and Otic ganglion