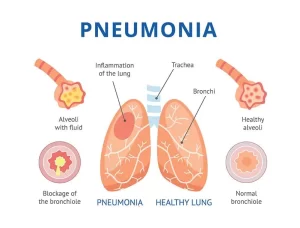
Inflammation of the lung parenchyma, What causes lung parenchyma?, Is lung parenchyma dangerous
Inflammation of the lung parenchyma is an acute lower respiratory infection associated with recently developed radiological signs. It is a condition where the functional tissues of the lungs, including the alveoli and surrounding structures, become inflamed. This can interfere with the lungs‘ ability to facilitate gas exchange.
Inflammation of the lung parenchyma
Inflammation of the lung parenchyma (the functional tissue of the lungs involved in gas exchange) is medically referred to as pneumonitis or, when caused by an infection, pneumonia. Pneumonitis is a general term for inflammation of the lung tissue, often caused by non-infectious factors, such as allergens, irritants, or radiation. Pneumonia is Inflammation of the lung parenchyma caused by infectious agents like bacteria, viruses, or fungi.
Classification
1. Aetiological
• Infectious:
- Bacterial: a) Anaerobic, Intra cellular, T.B, gram +ve, gram-ve. b) Nocardia, Actinomyces, Typhoid.
- Viral: RSV-CMV-Influenza – Herpes
- Fungal
- Protozoal: Pneumocystic Carinii, Toxoplasma
- Rickettsial: Typhus – Q Fever
• Non-Infectious:
- Collagen diseases: Rheumatoid – SLE-Rheumatic fever.
- Chemical: Mendelson’s syndrome, Pneumonia Lipoid.
- Radiation pneumonia (End by fibrosis)
2. Radiological Classification:
- Lobar: Lobar or segmental consolidation.
- Bronchopneumonia: Bilateral patchy or lobular consolidation.
3. Recurrent Pneumonia
1) Local Bronchial obstruction:
- Intra luminal eg, foreign body.
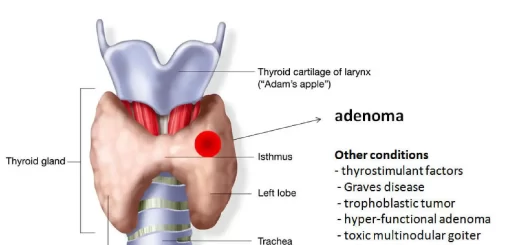
- Intramural stenosis eg Adenoma – Carcinoma-Stenosis.
II) Local Bronchopulmonary disease:
• Congenital e. g sequestration (separation of lobe of the lung). Localized Bronchiectasis, Carnified lung from chronic pneumonia.
III) Generalized Broncho-pulmonary disease:
- Bronchiectasis (infection with bad odor sputum and may be associated with hemoptysis).
- Cystic Fibrosis.
- COPD.
- Chronic sinusitis with postnasal drip (stagnation of secretion will be a good media for infection).
IV) Non-respiratory Causes:
- Epileptics-Neuromuscular-Esophageal-Alcoholics.
- Gingival disease
- Immune deficiency states
- CHF (Congestive Heart Failure)
4. Standard Clinical Classification:
- Community-Acquired Pneumonia (CAP).
- Hospital Acquired Pneumonia (Nosocomial).
Community-Acquired Pneumonia (CAP)
Pneumonia occurs in patients who have not been hospitalized or living in a nursing home during the 2 weeks prior to the onset of symptoms.
Pathogens
- Gram +ve bacteria: Streptococcus pneumoniae (30-40%). pyogenes, Staphylococcus pyogenes, Streptococcus aureus.
- Gram-ve bacteria: Hemophilus influenzae (2-11%), Moraxella catarrhalis (2%), Klebsiella, Pseudomonas, E. coli.
- Atypical (Intracellular) organisms: Legionella pneumophilia (1-16% Chlamydia Pneumonia (11-17%), Mycoplasma Pneumoniae (6-15%).
Complications of Pneumonia
- Thoracic complications: empyema, lung abscess
- Septic extra-thoracic complications: arthritis, cellulitis, pericarditis, endocarditis, meningitis, brain abscess
- Systemic complications: abnormal liver function tests, hemolytic anemia, circulatory failure, renal failure, thrombophlebitis, glomerulonephritis.
Hospital Admission
- High blood urea.
- WBC < 4000 or > 30000
- Serum albumin < 3.5 gm.
- Low PaO2.
- Multiple lobes involved in X-rays.
Diagnosis
- Clinical evaluation.
- Laboratory evaluation: (Routine blood chemistry, CBC, ESR, CRP, ABG).
- Radiographic evaluation: Confirm diagnosis and rule out complications.
- Microbiological evaluation: Gram stain, C. S. of sputum if: Drug-resistant pathogen is suspected, and Organisms not covered by empiric therapy are suspected. Pleural fluid and blood Culture.
- Serologic testing: for atypical bacteria and viruses.
- Urinary antigen: for legionella pneumonia and streptococcus pneumonis.
- Invasive diagnostic techniques (bronchoscopy) especially if pneumonia is recurrent or non-resolving.
Even with intensive diagnostic testing, most investigators cannot identify a specific etiology for Community-Acquired Pneumonia in up to half or more.
CAP Management
Two rules are to be considered:
- It’s an empirical therapy according to guidelines till results of culture & sensitivity are available.
- All patients should be treated for the possibility of atypical infection,
Patient stratification: according to the following:
- Place of therapy.
- Outpatient.
- Inpatient ward.
- ICU.
- Presence of cardiopulmonary disease or comorbidity
- Presence of modifying factors.
Initial Treatment Strategies for Outpatients with Community-acquired Pneumonia
1. No comorbidities nor receipt of parenteral antibiotics in the last 3 months.
Advance generation macrolide e.g., Azithromycin. OR Doxycycline, Amoxicillin.
2. Patients with comorbidities or who received parenteral antibiotics in the last 3 months.
- A respiratory fluroquinolone e.g., Moxifloxacin 400 mg, Gemifloxacin 320 mg or Levofloxacin 750 mg daily.
- OR Beta-lactam (Amoxicillin-Clavulanic acid 2 gm twice daily) + Macrolide (Azithromycin or Clarithromycin).
3. In regions with a high rate of infection with high-level macrolide-resistant Streptococcus pneumoniae, consider the use of alternative agents listed above in (2) for patients without comorbidities.
Inpatient, non-severe pneumonia: (non-ICU)
- Parenteral administration of a respiratory Fluroquinolone
- OR Beta-lactam (Amoxicillin-Clavulanic acid) + Macrolide (Azithromycin or Clarithromycin).
- If there are risk factors for MRSA or aeruginosa, obtain a sputum culture.
ICU patient, with severe pneumonia
- Beta-lactam (Cefotaxime, Ceftriaxone, or Ampicillin-Sulbactam) + either Azithromycin or a respiratory fluoroquinolone.
- Add coverage for MRSA (Vancomycin or Linezolid) or P. aeruginosa if risk factors are available, and obtain culture to allow de-escalation or continuation.
Once the etiology of CAP has been identified based on reliable microbiological methods antimicrobial therapy should be directed at the pathogen.
Duration of therapy
- Minimum 5 days.
- Afebrile for 48-72 h.
- Should have no more than 1 CAP-associated sign of instability before discontinuation of therapy.
Clinically stable: (Criteria for switch to oral therapy or discharge)
- Temp <37.8.
- HR 100 beats/m.
- RR 24 breath/m.
- Sys BP > 90 mmHg.
- O2 sat > 90%.
- Ability to maintain oral intake.
- Normal mental status.
Response to therapy
- Fever → 2-4 days.
- Leukocytosis →4 days.
- Crackles → 7 days.
- X-ray → weeks.
Causes of Inflammation of the lung parenchyma
Infectious Causes (Pneumonia):
- Bacterial: Streptococcus pneumoniae, Haemophilus influenzae, Legionella pneumophila.
- Viral: Influenza virus, SARS-CoV-2 (COVID-19), Respiratory Syncytial Virus (RSV).
- Fungal: Aspergillus, Histoplasma, Cryptococcus.
Non-Infectious Causes (Pneumonitis):
- Allergic Reactions: Hypersensitivity pneumonitis from exposure to mold, bird feathers, or other allergens.
- Environmental Irritants: Inhalation of chemical fumes, dust, or smoke.
- Radiation Therapy: Radiation pneumonitis as a side effect of cancer treatment.
- Autoimmune Conditions: Conditions like sarcoidosis or lupus.
- Drug-Induced: Certain medications, such as chemotherapy agents or immune checkpoint inhibitors.
Symptoms
General Symptoms:
- Cough (may be dry or productive).
- Shortness of breath (dyspnea).
- Fatigue.
- Chest pain (often pleuritic).
- Fever (common in infections).
Severe Symptoms:
- Rapid breathing or difficulty breathing.
- Cyanosis (bluish discoloration of lips or skin).
- Confusion (especially in older adults).
Diagnosis
Clinical Examination: Listening to lung sounds with a stethoscope (crackles, wheezing, or diminished breath sounds).
Imaging:
- Chest X-ray: Shows infiltrates or areas of opacity.
- CT Scan: Provides more detailed images of lung tissue and patterns of inflammation.
Laboratory Tests:
- Blood Tests: Assess markers of infection (e.g., WBC count, CRP, procalcitonin).
- Microbial Tests: Sputum culture, blood culture, or PCR for viruses.
- Lung Biopsy: In rare cases, to identify non-infectious causes.
Pulmonary Function Tests: Assess lung capacity and gas exchange, particularly in chronic pneumonitis.
Treatment
Infectious Causes (Pneumonia):
- Antibiotics: For bacterial infections (e.g., amoxicillin, azithromycin).
- Antiviral Drugs: For viral causes like influenza or COVID-19.
- Antifungal Therapy: For fungal pneumonia (e.g., amphotericin B, fluconazole).
Non-Infectious Causes (Pneumonitis):
- Corticosteroids: To reduce inflammation (e.g., prednisone).
- Immunosuppressive Therapy: For autoimmune-related conditions.
- Avoidance of Irritants: Eliminate exposure to allergens or harmful chemicals.
- Supportive Care: Oxygen therapy, bronchodilators, or pulmonary rehabilitation.
Complications
- Respiratory failure.
- Pulmonary fibrosis (scarring of lung tissue).
- Sepsis (in cases of severe infection).
- Chronic obstructive pulmonary disease (COPD) exacerbations.
You can subscribe to Science Online on YouTube from this link: Science Online
You can download Science Online application on Google Play from this link: Science Online Apps on Google Play
Hospital-Acquired Pneumonia symptoms and treatment, What is the difference between HAP and VAP?
Pneumonia causes, types, treatment, Is pneumonia usually serious? and Is pneumonia contagious?
Chronic Obstructive Pulmonary Diseases Treatment, Types and Causes of COPD
Steps of Asthma control, What is good control of asthma? and What is asthma management?
Spirometry uses, What is a normal spirometry level? and What is FEV1 in spirometry?
Lung structure, borders, Lobes, Fissures, and Broncho-pulmonary segments
Larynx structure, function, cartilage, muscles, blood supply, and vocal folds
Anatomy of the nose, function of para-nasal air sinuses, and Sphenopalatine Ganglion branches
Thoracic vertebrae structure, function, Chest wall muscles, and Intercostal arteries
Diaphragm anatomy, structure, function, Phrenic nerves, and Nerves of the thorax