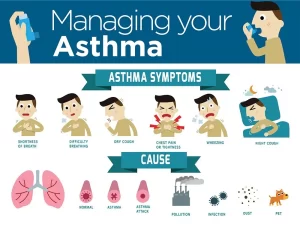
Steps of Asthma control, What is good control of asthma? and What is asthma management?
Asthma control refers to managing and minimizing the symptoms of asthma to maintain a normal lifestyle and reduce the risk of asthma attacks or exacerbations. Proper asthma control involves a combination of medication, lifestyle management, and environmental control.
Assessing Asthma Control
Asthma control indicates the extent to which the effects of asthma can be seen in the patient or have been reduced or removed by treatment.
Asthma control includes:
- Symptom control is established through the application of a simplified scheme for recognizing the level of asthma control (controlled, partly controlled. and uncontrolled asthma).
- Risk factors are factors that increase the patient’s future risk of having exacerbations (flare-ups), loss of lung function, or medication side effects. Risk factors are assessed at diagnosis and periodically.
- Measure lung function can measure FEVI1% before starting treatment, 3-6 months later, and then periodically, e.g., yearly. Lung function is most useful as an indicator of future risk.
Assessing the severity of the underlying disease
The degree of symptoms, airflow limitation, and lung function variability have allowed asthma to be classified by severity into:
- Intermittent-Mild Persistent,
- Moderate Persistent-Severe Persistent.
Management of bronchial asthma
Long-term management “In between acute attacks”
The long-term goals of asthma management are symptom control and reduction of risk of exacerbations, airway damage, and medication side effects
These goals can be achieved by:
- Medications: Every patient with asthma should have a reliever medication, and most patients with asthma should have a controlled medication.
- Treating modifiable risk factors and co-morbidities eg, smoking, anxiety, depression, rhinitis, sinusitis, GERD.
- Non-pharmacological therapies and strategies.
Pharmacological therapy includes
1. Reliever drugs: (relive bronchospasm)
- Short-acting inhaled beta 2 agonists (SABA).
- Anticholinergics.
- Methylxanthines.
- Short-acting oral beta 2 agonists.
2. Controller drugs: {to control airway inflammation)
- Corticosteroids: systemic and inhaled.
- Long-acting inhaled beta 2 agonists (LABA).
- Leukotriene-receptor antagonists or Lipo-oxygenase inhibitors.
- Nedocromil Sodium & Cromolyn Sodium.
- Methylxanthines.
- Long-acting oral beta 2 agonists.
- Long-acting inhaled anticholinergic (tiotropium).
- Anti-lg E (omalizumab).
- Anti-IL5 (mepolizumab).
Control-based asthma management
Stepwise approach for adjusting treatment (GINA 2016 report for adults, children 12 years)
Once asthma treatment has been started, ongoing decisions are based on a cycle to:
- Assess (Level of symptom control, risk factors, pulmonary function).
- Adjust treatment.
- Review response to treatment.
The preferred treatments at each step are based on severity and level of asthma control, Inhaled SABAs are medications of choice for quick relief of asthma symptoms and bronchoconstriction, SABAs should be used only as needed at the lowest dose and frequency required, Tremor and tachycardia are commonly reported side effects with the initial use of SABA. Excess use or poor response indicates poor asthma control.
For the best outcomes, regular daily controller treatment should be initiated as soon as possible after the diagnosis of asthma is made. Long-acting anticholinergic (tiotropium): An add-on option at Step 4 or 5 by mist inhaler for patients >12 years with a history of exacerbations despite ICS ± LABA.
Anti-IgE (omalizumab): An add-on option for patients with severe persistent allergic asthma uncontrolled on Step 4 treatment (high dose ICS/LABA), Anti-IL5: An add-on option for patients aged >12 yrs with severe eosinophilic asthma uncontrolled on Step 4 treatment (high dose ICS/LABA).
Reviewing response and adjusting treatment after starting initial controller treatment
Patients should preferably be seen 1-3 months after starting treatment or according to clinical urgency and every 3-12 months after that except in pregnancy when they should be reviewed every 4-6 weeks.
Consider stepping down when asthma has been well-controlled for 3 months + low risk for exacerbation, Consider stepping up if…. uncontrolled symptoms, exacerbation, or risk, but check diagnosis, inhaler technique, and adherence first.
Non-Pharmacological therapy
- Education.
- Avoidance of triggers.
- Smoking cessation advice.
- Influenza vaccination.
- Allergen Immunotherapy.
Asthma Exacerbation (acute asthma, asthma attack)
- Exacerbation is an acute or sub-acute worsening in symptoms and lung function from the patient’s usual status.
- Exacerbation severity is graded into mild, moderate, severe, and very severe (life-threatening).
- Criteria for exacerbation severity are based on symptoms, physical examination parameters, as well as lung function and oxygen saturation.
- Grading of severity is essential to provide the appropriate management regarding site (primary or acute care, ICU) and plan of treatment.
Clinical presentation
- In 85-90% of life-threatening asthma presents after several days of worsening symptoms and often occurs in patients with severe and poorly controlled asthma, In 10%, the onset is more rapid, and asthma progresses over minutes to hours.
- Patients with acute severe asthma are dyspneic (talks in words), agitated, and diaphoretic, typically sitting upright, tachycardic (pulse rate >120/ min), and tachypneic (RR>30/min), using accessory muscles, O2 saturation on room air <90%, PEF <50% of predicted.
- In Life-threatening asthma patients (more advanced stage) become drowsy. confused, may have a silent chest, bradycardia, and hypotension.
- Physical examination reveals diffuse wheezing or, if air movement is poor, no breath sounds at all (silent chest). The severity of wheezing correlates poorly with the degree of obstruction.
Arterial blood gases
- Hypoxia tends to be modest and can easily be overcome by supplemental oxygen.
- Early in the presentation, hypocapnia reflects compensatory hyperventilation.
- Normal or increased CO2 implies severe disease.
- A steadily rising PaCO2 reliably indicates impending respiratory failure and the need for mechanical ventilation.
- Lactic acidosis (metabolic acidosis) is due to hypoxia, increased production by respiratory muscles, reduced lactate clearance due to circulatory failure or induced by b2 agonists. Lactic acidosis should be considered a marker of severe disease.
Management of acute severe asthma
- Management of acute severe asthma usually requires emergency department visits and likely hospitalization and even ICU admission.
- The goals of treatment are correction of hypoxemia and rapid reversal of airflow.
- obstruction is best achieved by oxygen administration and repetitive treatment with short-acting beta 2 agonists.
- Early use of systemic corticosteroids can reduce the risk of relapse.
A. Oxygen therapy
Administration of oxygen via mask, or nasal cannula with flow rates adjusted to maintain oxygen saturation of 93-95% in adults and adolescents (94-98% in children 6-12 years).
B. Bronchodilators
1. Short-acting beta 2 agonists (SABA):
- Inhaled short-acting beta2 agonist treatment is the mainstay of treatment for acute asthma.
- Treatment must be given frequently and in high doses, delivered either with an MDI and spacer or via nebulization.
- 2.5-5 mg of albuterol via an oxygen-driven nebulizer every 20 min (up to three times).
- Or 4 to 6 puffs of albuterol every 20 min using an MDI/spacer.
- Or Continuous nebulization at 10 mg/hour driven by oxygen.
- Higher inhaled doses may be required in mechanically ventilated patients due to aerosol losses in the ventilator.
- Most patients respond within 1 hour of treatment.
- Monitor treatment response after 1 hour or earlier (improvement of PEF or FEV2, symptoms).
- If the patient is improving continue nebulized β2 agonist and ipratropium 4-6 hourly.
2. Inhaled Anticholinergics
- For patients with acute severe or life-threatening asthma add nebulized Ipratropium bromide (0.5 mg) or 4 to 10 puffs by an MDI/spacer to beta 2 agonist treatment every 20 minutes (up to 3 times), thereafter, they are given 4-6 hourly.
- This combination has been shown to produce significantly greater bronchodilatation than β2 agonist alone.
In patients who have a poor response to inhaled bronchodilator therapy (β2 agonist & ipratropium bromide) add magnesium sulphate.
3. Magnesium sulphate
- In patients who have a poor response to inhaled bronchodilator therapy (beta 2 agonist & ipratropium bromide) add magnesium sulphate.
- It is usually given a 1.2-2 g IV infusion over 20-30 minutes.
4. Theophylline
- At therapeutic doses, methylxanthines are weaker bronchodilators than beta-agonists and have many undesirable adverse effects.
- Although its use is controversial, theophylline may help some patients who are not responding to high-dose albuterol and steroids.
- The loading dose is 5mg/kg load can be given over 30 minutes, followed by a maintenance dose of 0.4 mg/kg/h.
- Blood level monitoring is recommended. (Therapeutic level between 10-20 mg/dL).
C. Systemic corticosteroids
- Short-term treatment (usually 5-7 days in adults) is important early in the treatment of severe acute exacerbations, with the main effects seen after 4-6 hours.
- Oral corticosteroid (OCS) therapy is preferred and is as effective as IM or IV therapy in preventing relapse.
- The dose of oral prednisone is 40-50 mg/day in 1 or 2 divided doses.
- IV hydrocortisone 100 mg /6 hours is given for patients with absorption problems or those who are not able to take orally due to the severity of their respiratory distress, or mechanically ventilated.
Inhaled corticosteroids
Several recent studies assessing the role of inhaled corticosteroids in acute asthma suggest that a combination of high-dose inhaled corticosteroids with inhaled salbutamol provided greater bronchodilatation than inhaled salbutamol alone.
Adjunct Therapy
- Heliox.
- IV Leukotriene receptor antagonists e.g. monteleukast.
- Anaesthetics e.g. Inhaled lidocaine, IV propofol & ketamine.
Antibiotic therapy: It is not routinely indicated for patients with acute severe asthma unless pneumonia or other evidence of bacterial infection is present.
Monitoring
- Repeat measurement of PEF 15-30 minutes after starting treatment.
- Oximetry.
- Repeat blood gas measurements within 1 hour of starting treatment if Initial Pa02 <60 mmHg. PaCG2 normal or raised, Patient deteriorates.
D. Mechanical Ventilation
A. Non-Invasive Positive Pressure Ventilation (NPPV);
NPPV is applied in alert, cooperative patients with acute severe asthma who do not respond adequately to medical therapy. NPPV improves ventilation/perfusion mismatch, decreases the work of breathing, resting the diaphragm and inspiratory muscles, and reduces the need for endotracheal intubation.
NPPV is contraindicated in patients with decreased levels of consciousness excess respiratory secretions, severe hypoxia, or hypercapnia PaCO2 > 60 mmHg, hemodynamic instability, and poor patient cooperation.
B. Intubation & Mechanical Ventilation
Indications:
- Refractory hypoxemia (PaO2 <60mmHg).
- Increasing hypercapnia (PaCO2 >5 mmHg/h).
- Signs of exhaustion despite bronchodilator therapy.
- Worsening of mental status.
- Hemodynamic instability.
- Coma or apnea.
Medications:
- Controller Medications: These are long-term medications taken daily to reduce airway inflammation and prevent symptoms. The most common controller medications are inhaled corticosteroids (ICS), which reduce inflammation in the airways over time.
- Examples: Fluticasone, Budesonide.
- Rescue Medications: These are short-acting medications taken during an asthma attack to quickly relieve symptoms like wheezing or shortness of breath. The most common are short-acting beta-agonists (SABAs), which relax the muscles around the airways.
- Examples: Albuterol, Levalbuterol.
Long-Term Asthma Management
- Regular Checkups: Regular visits to a healthcare provider (typically every 3-6 months) ensure that asthma is well-managed, medications are adjusted as needed, and lung function is monitored.
- Environmental Modifications: Making adjustments to the home and work environment, such as using air purifiers or allergy-proof bedding, can help reduce exposure to asthma triggers.
You can subscribe to Science Online on YouTube from this link: Science Online
You can download Science Online application on Google Play from this link: Science Online Apps on Google Play
Spirometry uses, What is a normal spirometry level? and What is FEV1 in spirometry?
Lung structure, borders, Lobes, Fissures, and Broncho-pulmonary segments
Larynx structure, function, cartilage, muscles, blood supply, and vocal folds
Anatomy of the nose, function of para-nasal air sinuses, and Sphenopalatine Ganglion branches
Thoracic vertebrae structure, function, Chest wall muscles, and Intercostal arteries
Diaphragm anatomy, structure, function, Phrenic nerves, and Nerves of the thorax