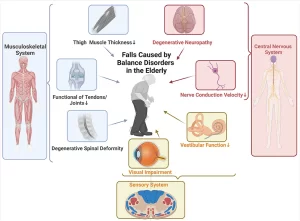
Causes of Falls in the elderly, How to prevent falls and why do the elderly die after a fall
Falls in the elderly are a notable problem among the elderly and cause injury and hospitalization. Understanding the causes, risks, and prevention strategies is crucial to improving health outcomes and maintaining independence for older adults. Several risk factors contribute to falls in the elderly, and understanding these can help in preventing falls and reducing injury risks.
Causes of Falls in the Elderly
- Decreased muscle strength in the legs and core makes balance difficult.
- Age-related changes in balance can increase the risk of falls.
- Poor eyesight from conditions like cataracts or glaucoma affects depth perception and mobility.
- Many conditions such as arthritis, Parkinson’s disease, and diabetes can impair mobility.
- Some medications can cause dizziness, drowsiness, or hypotension, increasing fall risk.
- Loose rugs, poor lighting, and cluttered pathways can lead to trips and falls.
- Wearing shoes that don’t provide adequate support or traction increases the risk of slipping.
- Stairs without railings or uneven floors present a challenge.
- Once someone has fallen, fear of falling again can lead to reduced activity, weakening muscles, and further increasing fall risk.
- Dementia or other cognitive impairments may cause difficulty in navigating or perceiving environmental risks.
Risks Associated with Falls
- Hip fractures are especially common and often result in a long recovery or reduced mobility.
- Falls can lead to traumatic brain injuries, especially in individuals taking blood thinners.
- Falls often lead to extended hospital stays, rehabilitation, and a potential decline in overall health.
- A serious fall can lead to long-term care needs or moving to assisted living facilities.
Prevention Strategies
- Regular physical activity improves muscle strength, flexibility, and balance. Tai Chi, yoga, and strength training are effective fall-prevention exercises.
- Periodically reviewing medications with a healthcare provider can identify those that may increase fall risk.
Home safety modifications
- Installing grab bars in the bathroom.
- Improving lighting throughout the home.
- Removing tripping hazards like rugs or electrical cords.
- Installing railings along stairs and using non-slip mats.
- Regular eye exams and hearing tests can help detect changes that could lead to falls.
- Encouraging the use of well-fitting, supportive shoes with non-slip soles can help prevent slips and trips.
After a Fall: Recovery and Support
If a fall occurs, it’s important to assess the situation carefully:
- Immediate medical attention may be required, especially if there’s pain, a visible injury, or unconsciousness.
- Physical therapy can help restore mobility and strength, reducing the likelihood of future falls.
- Support systems, such as having emergency alert devices or family check-ins, provide peace of mind and faster response if another fall occurs.
- Preventing falls in the elderly requires a proactive approach that involves physical health, environmental adjustments, and awareness.
Falls in the elderly
Nonsyncopal falls unintentional events in which a person comes to rest on the floor or ground that are not caused by loss of consciousness, stroke, seizure, or overwhelming force.
- Falls have multifactorial etiology.
- They can be prevented by treating the factors that increase an older person’s risk of falling.
- Effective treatment requires a multidisciplinary approach.
- Few specialized fall centers around the world.
- Perhaps because of this, fall prevention is not widely practiced in clinical settings outside of specialized geriatric assessment clinics.
Example:
A 74-year-old man with type 2 DM, peripheral neuropathy, IHD, OA, diminished visual acuity, and dementia.
He needs:
- Geriatric med. To control medical conditions.
- Orthopedist For Advanced OA.
- Ophthalmologist For vision
- ENT For Hearing.
- Geriatric neuropsychiatric For Dementia.
Integration
Physiotherapists, geriatric nurses, and occupational therapists help train weak muscles, and sensations, increase cooperation, and how to move with OA joints.
Incidence
- Approximately 40% of persons aged 65 years and over fall in a given year, and half of persons who fall do so more than once.
- The incidence increases steadily after the age of 60 years.
- The rates for falls in nursing facilities and hospitals are more common than for community-dwelling elders and are estimated at 1.5 falls per year.
- Women are more likely to fall than men.
Complications of falls
Hip fractures
Hip fractures are probably the most dreaded fall-related injury as approximately half of older persons who sustain a hip fracture cannot return home or live independently after the fracture, and up the fracture, and up to 20% die within a year of the fracture.
- Lacerations.
- Serious soft-tissue injuries.
- head trauma.
- fear of falling again.
- loss of physical function and independence.
- falls and fall injuries are major determinants of nursing home placement.
- long lies with the risk of pneumonia, dehydration, rhabdomyolysis, and hypothermia.
Long lie
It is defined as remaining on the ground for greater than one hour after a fall. persons are often unable to get up from the ground or floor after a fall.
Complications of a long lie
- pneumonia.
- rhabdomyolysis (dissolution of muscle fibers).
- dehydration.
- hypothermia.
Rhabdomyolysis
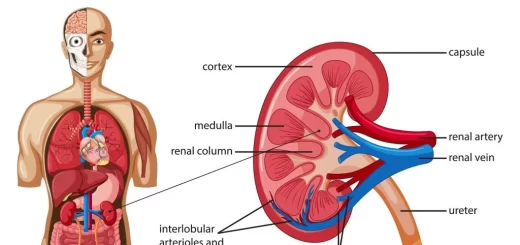
- It is a clinical syndrome ranging from isolated raised CK to acute kidney injury (AKI), hyperkalemia, and death.
- Rhabdomyolysis results in the leakage of potassium, phosphate, myoglobin, and creatine kinase (CK) into the circulation.
- Myoglobulinuria can be screened for in the ED (emergency department) with simple urine analysis by dipstick test which reads positive for haemoglobin if myoglobulinuria is present.
- Acute kidney injury (AKI): due to myoglobin causing renal tubular obstruction. Treatment is prompt aggressive IV rehydration, bladder catheterisation, and monitoring of urine output aiming for 200-300 ml/he
- Caution: In patients with known heart failure, fluid resuscitation must be carefully balanced. The longer it takes for fluid resuscitation to start the more likely AKI will develop. In patients whose renal function is Not responding to IV rehydration a period of renal replacement therapy is needed.
- Hyperkalemia: due to the direct release of potassium into the circulation, optimizing rehydration is essential in the management. Emergency treatment with calcium gluconate and an insulin-dextrose infusion may also be required. Arrhythmias are more common in patients with cardiac comorbidity.
- Hypocalcemia: Often asymptomatic, but parenteral calcium replacement should be administered if there is significant derangement.
Any elderly lying on the floor for an uncertain period should be considered a Long lie and should be evaluated for complications.
Hypothermia
Core body temperature:
- Mild < 35 C: The patient is fully conscious, alert, and shivering ( no bradycardia), keep the patient dry, use warm blankets and hot drinks.
- Moderate < 32 C: The patient seems apathetic (weakness with no shivering).
- Severe < 28 C:
Moderate and Severe cases need Intensive Care Admission.
Post fall syndrome
- The term post-fall syndrome was first proposed by Murphy & Isaacs in 1982 when they reported a peculiar reaction of the elderly after they had had a fall.
- patients expressed great fear of falling when they stood erect, tending to grab and clutch at objects within their view, and showing remarkable hesitancy and irregularity in their walking attempts.
- So gross were these signs and so related to the history of recent falls, that the term (post-fall syndrome) was proposed to describe the picture.
- The post-fall syndrome was subdivided into severe – moderate – absent.
Severe type
where severe syndrome was said to be present when following a fall, the patient was:
- Unable to stand or to walk unsupported when asked to do so.
- Assumed an expression of fear and anxiety clutched to any object within the field of vision staggered.
- Stumbled or rushed forward and appeared to be in imminent danger of falling. (and in the absence of any neurological or orthopedic abnormality which in itself may adversely influence gait and balance).
When these pts were provided support their behaviour was modified and a fairly normal pattern of stepping took place.
Moderate type
In the moderate degree of the syndrome the pt. presented features of anxiety, hesitancy, and tendency to clutch and grab but with encouragement was able to stand and walk without support.
Absent type
the syndrome was said to be absent when the pt was able to walk safely without human support and without any tendency to clutch and grab with or without a walking aid.
“Ptophobiae. the phobic reaction to standing or walking was largely believed to be a consequence of falling resulting from the psychological trauma of the fall. Recent research has shown that this fear occurred also in elderly persons who have Not fallen before!!
The term Fear of Falling (FOF) is now being used and is defined as an ongoing concern about falling that ultimately limits the performance of daily activities. The term “FOF” is now used to encompass both fallers and non-fallers.
Other systematic reviews and research studies have come up with the following conclusions:
- FOF occurs both in fallers and Non-fallers. It is not only a postfall reaction.
- FOF is associated with a decline in physical health and balance impairments (e.g. osteoarthritis, visual impairments, general perception of poor health) It is not a result of normal aging.
- FOF is associated with (but Not only due to) anxiety and depression.
- FOF is associated with restricted activity, a sedentary lifestyle, and a lack of social interaction and support.
- FOF may be a more serious problem than falls in older adults.
Complications of Immobility
- Skin → Pressure ulcer.
- Muscles → Atrophy (one day after complete bed rest).
- Bones→Resorption and osteoporosis.
- Joints→ Stiffness, Pain, and Contractures.
- CVS→ ↓ COP, Orthostatic hypotension, Venous thromboembolism.
- Pulmonary→ Pneumonia.
- GIT→ Constipation.
- Urinary→ Urinary tract infection.
- Decreased BMR.
You can follow science online on YouTube from this link: Science online
You can download Science Online application on Google Play from this link: Science online Apps on Google Play
Urinary incontinence in elderly causes and treatment, How to correct urinary incontinence?
Properties of cardiac muscles, Cardiac automaticity, and Conduction of electrical impulses
Histology of the heart, Cardiomyocyte types, Ultrastructure, and features of cardiac muscle fibers
Mediastinum contents, Aorta parts, Brachiocephalic trunk, Pulmonary trunk, and Thoracic duct trunk
Electrocardiogram (ECG) importance, ECG test results, analysis and abnormalities
Heart and Pericardium structure, Abnormalities, and Development of the heart
Heart function, structure, Valves, Borders, Chambers and Surfaces
Cardiac Markers review, definition, list, test, and myoglobin function