Principles of drug use and Effective Treatment, High-risk drugs and How to reduce medication errors
Principles of drug use refer to a set of guidelines aimed at ensuring that the use of drugs, whether medicinal or recreational, is done safely, ethically, and with an understanding of the consequences. These principles can be categorized into medical, social, and legal contexts.
Principles of Drug Use
- Ask: Is treatment warranted?
- Are non-pharmacologic alternatives available?
- Consider the risk vs. benefit of drug therapy.
- You should establish goals of therapy: Quality of care, Quality of life, and Functional status.
- You have to consider the whole person, not just one disease or one drug.
- You should be aware of the assumptions behind clinical practice guidelines.
- The disease management may not be adequate or appropriate if multiple chronic diseases are present.
Rational Drug Prescribing in Elderly
Purpose:
- You should determine whether underuse, overuse, or misuse is a problem.
- Prescribe the most effective drug.
- Minimize the side effects and risks of iatrogenic harm.
- Maximize compliance and adherence.
- Conserve resources through intelligent prescribing.
Appropriateness:
The potential benefits outweigh the potential risks which is different from Polypharmacy which means concurrent use of many medications.
Rational prescribing
- You have to determine if the drug is needed or not.
- Indeed, review all drugs to see if they are still needed.
- If the drug is needed, assess the patient for frailty and co-morbidities, review prior and current medications, and asses the patient’s ability to comply with directives.
- Pick a drug and dose based on your knowledge of the patient and the drug.
- Use explicit criteria (software, lists, other tools) to evaluate choices, drug interactions, and drug-disease interaction.
- When uncertain, consult with a knowledgeable pharmacist.
- Explain the drug use to the patient: Written directives are the best, and use the opportunity to enhance compliance.
- Monitor for effectiveness and side effects.
- Re-evaluate the need for ongoing therapy.
Guidelines for optimal pharmacotherapy
- Obtain a complete drug history about all the medications the patient is taking as well as previous treatments and responses or allergies.
- Ask about the patient’s habits as alcohol, tobacco, and caffeine.
- Every visit Review medications to stop drugs that are no longer needed, and if you need to prescribe new drugs.
- Monitor the use of OTC drugs.
- Avoid prescribing before a diagnosis is made.
- Use non-pharmacologic approaches whenever possible.
- You should know the actions, adverse effects, and toxicity profiles of the medications you prescribe.
- Choose once-daily formulations.
- You have to use one drug to treat two or more conditions.
- Start the drug therapy at a low dose and titrate the dose according to tolerability and response, reach the therapeutic dose before switching or adding another drug.
- If you need more than one drug, Use combination products cautiously.
- You should avoid medications with common side effects.
- Avoid using a drug to treat the adverse events caused by another.
- Encourage the use of a pillbox to avoid confusion.
- You should avoid using drugs from the same class or with similar actions.
- Inquire about side effects from prescriptions regularly.
- Identify compliance of the patient.
- Educate the patient and/or caregiver about each medication regarding the regimen, the therapeutic goal, the cost, and potential adverse effects or drug interactions. Provide written instructions.
How to reduce medication errors
- Know well about the medication’s dose, adverse events, interactions, and monitoring.
- Write the drug’s name right to avoid misreading.
- You should write out the directions, strength, route, quantity, and number of refills.
- Avoid abbreviations as qd, and ud.
- Try to write the diagnosis for which the drug is prescribed.
- Always re-read what you’ve written.
Recommendations for pharmaco-therapy in geriatric patients
- Is pharmacotherapy necessary?, a clear diagnosis, non-pharmacological possibilities.
- Well-documented pharmacotherapy, avoid new drugs and drugs with long half-life.
- Avoid polypharmacy.
- Start low, go slow.
- Consider unusual side effects.
- Always answer the following questions:
- can a drug be stopped? unprescribing or „pruning” of drug regimen.
- does the patient understand the therapy?
- Is the patient able to follow the therapy?
Principles of Prescribing for the Elderly
1. Start low
- Published starting doses may be based on tests for younger people.
- Promotes early identification of side effects.
2. Consider risks vs. Benefits
- Side effects may outweigh the benefits.
- Don’t prescribe one drug to address the side effects of another.
3. Consider preexisting medical conditions
- Some drugs may worsen existing conditions.
- For example arthritis meds and kidney disease.
4. Consider the risk of drug interactions
- Watch out for anticoagulants.
- Use existing information.
- Risk increases with several drugs.
5. Use as few drugs as possible
- Age and number increase the risk of adverse drug events.
- Competition in absorption or metabolism.
6. Consider dosage requirements
- Decrease in renal function.
- Metabolism changed by other drugs.
7. Consider effects on quality of life
- May cause change in social activities.
- The patient may not tell the doctor she has quit the med.
8. Use familiar agents
- Rarely a truly unique drug becomes available.
- With wide usage previously unknown side effects appear.
9. Consider the financial impact
- Many do not have insurance.
- New, marketed drugs are the most expensive.
- Consider alternatives.
- Use existing information
10. Obtain a drug-free interval
- Seek past medical records.
- May discontinue some drugs with close follow-up.
11. Define outcomes for therapy
- What are we trying to fix?
- Is this patient-oriented?
- Delete drugs that don’t meet the benefit.
12. Consider non-pharmacologic therapies
- Tai Chi for falls.
- Physical therapy for arthritis.
- Biofeedback for urinary incontinence.
13. Listen to your patient
- Be open to feedback.
- Ask if they can afford it.
- Encourage them to discuss decisions about meds and costs.
- Believe in uncommon side effects.
- Give more options.
Drug-disease interactions and high-risk drugs
Common drug-disease interactions
- Congestive Heart Failure → CCB & non-selective B-blockers.
- Diabetes Mellitus → Corticosteroids & ẞ- blockers.
- COPD and Asthma → Sedative-Hypnotics & ẞ- blockers.
- Peptic ulcer → NSAIDs & Corticosteroids.
- Seizures → Neuroleptics.
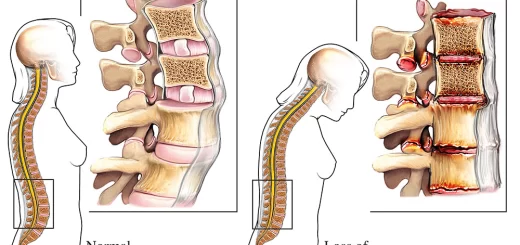
- Osteoporosis → Corticosteroids, Anticonvulsants.
- Clotting Disorders → NSAIDs, Teclopidine, Warfarin
- BPH → Anticholinergics & Antihistamines.
- Incontinence → Alpha Blockers.
- Constipation → Anticholinergics, Antihistamines, antispasmodics, Narcotics, CCB, Iron.
- Arrhythmia → TCAD
- Insomnia → Decongestants, Beta agonists.
- Cognitive dysfunction → Antispasmodics, Anticholinergics, Antihistamines.
High-Risk Drugs for the Elderly
- Warfarin.
- Digoxin > 0.125/day.
- Meperidine.
- Ticlodipine.
- Antihistamines (esp Diphenhydramine-Benadryl!).
- Chlorpropamide.
- NSAIDS (esp indomethacin).
- Propoxyphene.
Drugs to be avoided in the elderly
- Benzodiazepines such as Diazepam.
- Barbiturates.
- Analgesics such as NSAIDs.
- Muscle relaxants.
- Antiemetics-Prokinetics such as Metoclopramide.
- Antihistamines.
- Antidepressants and Combination antidepressant-antipsychotics.
- Anticholinergic antispasmodics.
- Cardiovascular drugs such as Methyldopa, Reserpine, Propranolol, and Digoxin.
In Summary For Elderly Patients
- Obtain a complete medication history.
- You should review medications regularly and before prescribing a new medication.
- Know the actions, adverse events, and toxicity profiles of prescribed medications.
- Start long-term medications at a low dose and titrate dose based on tolerability and response.
- You should attempt to reach a therapeutic dose before switching medication to or adding another medication.
- You have to educate the patient/ and/or caregiver about each medication.
- Avoid using one medication to treat the adverse events caused by another.
- Attempt to use one medication to treat 2 or more conditions.
- You should avoid using drugs from the same class or with similar actions.
- Communicate with other prescribers.
- You have to be knowledgeable about the medication’s dose, adverse events, interactions, and monitoring.
- You should write out the directions, strength, route, quantity, and number of refills
- Start low.
- Go slow (But get to therapeutic levels).
You can follow science online on YouTube from this link: Science online
You can download Science Online application on Google Play from this link: Science online Apps on Google Play
Properties of cardiac muscles, Cardiac automaticity and Conduction of electrical impulses
Histology of the heart, Cardiomyocyte types, Ultrastructure and features of cardiac muscle fibers
Mediastinum contents, Aorta parts, Brachiocephalic trunk, Pulmonary trunk and Thoracic duct trunk
Electrocardiogram (ECG) importance, ECG test results, analysis and abnormalities
Heart & Pericardium structure, Abnormalities, and Development of the heart
Heart function, structure, Valves, Borders, Chambers and Surfaces
Cardiac Markers review, definition, list, test, and myoglobin function