Drug use and prescribing for the elderly, Most common medications used in nursing homes
Effective prescribing for elderly patients requires careful consideration of the individual’s health status, drug interactions, and aging-related physiological changes. A personalized approach, regular medication reviews, and a focus on minimizing unnecessary medications can improve outcomes and reduce risks.
Drug use and prescribing for the elderly
Prescribing and managing drug use in the elderly require special attention due to age-related changes in the body and the higher likelihood of multiple medical conditions, Some key considerations include:
1. Physiological Changes in Aging
- The liver’s ability to metabolize drugs decreases with age, which can lead to the drug staying in the body longer and potentially causing toxicity.
- Kidney function: Reduced renal clearance can slow the excretion of drugs, increasing the risk of drug accumulation.
- Body composition: Older adults typically have more fat and less muscle mass, affecting the distribution of fat-soluble and water-soluble drugs.
- The elderly may be more sensitive to certain drugs, like sedatives or blood pressure medications, due to changes in receptor sensitivity.
2. Polypharmacy
- Elderly patients often take multiple medications (polypharmacy) for various chronic conditions. This increases the risk of drug-drug interactions, side effects, and medication non-adherence.
- Managing multiple prescriptions can result in unintended interactions, especially if the patient is seeing multiple healthcare providers.
3. Common Issues in Drug Prescribing
- Physicians may prescribe more medications than necessary due to the complexity of treating multiple conditions, leading to a higher risk of adverse drug events.
- Some essential drugs, such as pain relief or anticoagulants, may be underprescribed due to concerns about side effects, despite their potential benefits.
- Certain medications are not recommended for older adults due to higher risks of adverse effects (e.g., long-acting benzodiazepines, anticholinergic drugs, and certain antihypertensives).
4. Adverse Drug Reactions (ADRs)
- Older adults are more vulnerable to ADRs due to physiological changes and polypharmacy.
- Common ADRs: Dizziness, confusion, falls, hypotension, and gastrointestinal disturbances. These can severely impact the quality of life and lead to hospitalization.
5. Medication Adherence
- Elderly patients with memory issues or dementia may struggle to adhere to medication regimens.
- Multiple medications with different dosing schedules can confuse patients and lead to non-adherence.
- The cost of medications may prevent some elderly individuals from filling their prescriptions or taking them as directed.
6. Special Considerations for Prescribing
- Start with the lowest effective dose and increase gradually, monitoring closely for side effects or interactions.
- Regular review: Medications should be regularly reviewed to assess their necessity and effectiveness, with deprescribing (removing unnecessary medications) as needed.
- Non-pharmacological alternatives: Whenever possible, consider non-drug treatments for conditions like insomnia, anxiety, or pain (e.g., physical therapy, behavioral therapies).
- Ensure that elderly patients and their caregivers understand the purpose, dosage, and potential side effects of each medication.
Commonly Prescribed Drugs for the Elderly
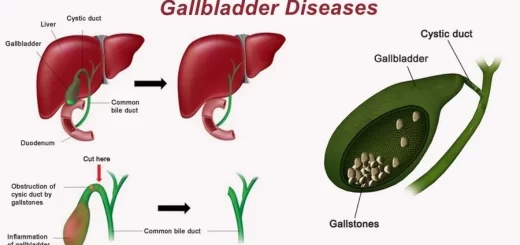
- Antihypertensives: To manage high blood pressure, but require careful monitoring to avoid hypotension and falls.
- Diabetes medications: Often used to manage type 2 diabetes, but dosing must be carefully controlled due to the risk of hypoglycemia.
- Pain medications: Opioids, NSAIDs, and acetaminophen are commonly used, but opioids can lead to addiction and NSAIDs can cause gastrointestinal or cardiovascular problems.
- Anticoagulants: Used to prevent strokes in patients with atrial fibrillation, but require close monitoring to avoid bleeding complications.
- Antidepressants and antipsychotics: Sometimes prescribed for depression or dementia-related agitation, but certain types (e.g., tricyclic antidepressants) can cause sedation, confusion, or increase the risk of falls.
Importance of geriatric drug therapy
- Aging of population.
- High use of drugs in the elderly.
- Prevalence of medication therapy problems.
- The shift from nursing facility to home and community-based services.
What is different about Geriatric Prescription?
- Underuse, Overuse, or Misuse problem?
- Altered Pharmacokinetics and Pharmacodynamics.
- Risk/Benefit Ratio in this vulnerable, frail population.
- The ability to recognize side effects in the elderly is reduced.
- Multiple physicians with poor communication among them.
- Compliance/Adherence considerations.
Medication Therapy Problems
- Polypharmacy: more than one drug use without indication.
- Undertreatment: indication without drug use.
- The dose is too low.
- The dose is too high.
- Adverse drug reaction.
- Drug interaction
- Inappropriate drug.
- Lack of adherence or compliance.
- Medication error.
Examples of Undertreatment
- Pain management.
- Pneumococcal and flu vaccine.
- Depression.
- Secondary heart attack prevention.
- Optimal use of medications in the elderly can be difficult and requires attention to the physiological changes that accompany aging.
- It is complicated by the fact that most elderly patients are on several medications at any given time.
- With increasing age and availability of more drugs, incidence of polypharmacy and inappropriate medication would be expected.
- The elderly population is a heterogeneous group, which means that the efficacy and toxicity of the same medication will vary widely from patient to patient.
- Adverse drug reactions and drug-drug interactions are more common in the elderly.
- Adherence to a prescribed regimen can often be difficult because of cognitive deficits, visual problems, financial difficulties, and complicated regimens.
Why do the elderly represent a therapeutic challenge?
Therapeutic Challenges
- Impaired Physiological Reserve in older patients “homeostenosis”.
- Multiple diseases (hypotension – IHD-Type 2 diabetes) and multiple drug use.
- Non-specific or cryptic presentation.
- Rapid deterioration if untreated (age-associated loss of adaptability).
- High incidence of complications (of disease and treatment).
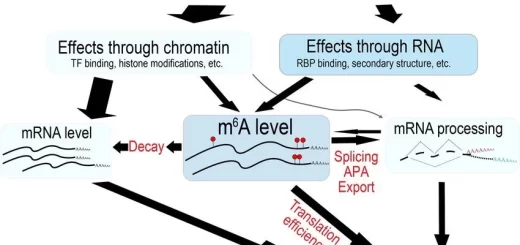
Altered Pharmacokinetics
- Absorption.
- Distribution.
- Metabolism.
- Clearance.
Absorption
- From a practical standpoint this is not usually a problem for the elderly.
- Caveat, Tube feedings may reduce absorption if continuous.
Distribution
In the elderly, this is significantly altered as a result of age-related changes in:
- Decreased muscle mass (sarcopenia)
- Decreased Thirst sensation→ Decreased total body water→ may cause Dehydration and it is the most important change, lower volume distribution of polar drugs.
- Decreased Bone mass
- Increased fat will increase the half-life of lipophylic drugs (e.g. diazepam, anesthetics).
- 5. Low serum albumin →changing the free vs. bound proportion of drugs.
Clearance (Kidney)
Clearance via Kidney is reduced
- Lower GFR (decreased in size, tubular secretion, and renal blood flow).
- Serum creatinine is not a reliable measure (it may be normal or slightly increased).
- Cockcroft-Gault is an estimate Renal (fx) shows big individual variations in the elderly.
- Creatinine Clearance (Cr cl.) (140-age) x body wt.(kg.)/( 72 x Serum Cr). (x 0.85 for Women).
Drugs with predominant renal elimination
- Aminoglycosides.
- Antimycotics: fluconazole, flucytosine.
- Antivirals: acyclovir, gancyclovir, ribavirin.
- Beta-blockers: atenolol, sotalol.
- Beta-lactam antibiotics: penicillins, cephalosporins.
- Digoxin.
- H2-Blockers.
- Lithium.
Metabolism (liver)
Drug Metabolism is Very Liver Dependent:
- Reduced liver function due to decreased liver size, blood flow, and disease (e.g. CHF).
- Phase I – first pass oxidative/reduction activities are reduced (e.g. (propranolol).
- Phase II drugs are preferred (oxazepam).
- In general, biotransforming enzymes are reduced in the elderly (eg. Cytochrome 450).
Altered Pharmacodynamics
- Alterations are complex and poorly studied.
- Generally the elderly are more sensitive to drug effects (e.g. the blood/brain barrier and anticholinergics and benzodiazepines) But, Beta-adrenergic effects are reduced.
- Homeostasis is more affected by drugs (e.g. postural BP, extrapyramidal system, thermoregulation, cognition).
Altered Pharmacodynamics
- Altered Pharmacodynamics – there are also important age-related changes in drug sensitivity (aging + drug-receptor interactions).
- Ageing is associated with an increased sensitivity for many compounds- opiates, and decreased B-adrenergic responses in the elderly (e.g., propanolol & isoproterenol).
Ageing is associated with changes in the end-organ responsiveness to drugs at the receptor or post-receptor level. Leading to ↓ sensitivity to certain drugs as ẞ-blockers and ↑ sensitivity to others as Warfarin.
Adverse Drug Events (ADE)
- Rate of ADEs requiring an ER visit for persons 65 and over is more than twice the rate for persons under age 65.
- Rate of ADEs requiring hospitalization is nearly seven times greater for persons age 65 or over versus persons under age 65.
- Any symptom in an elderly patient should be considered a drug side effect until proven otherwise.
- Adverse drug reactions represent the most common form of iatrogenic illness. 25% of hospitalized patients > 80 years experience an adverse drug reaction compared to 10% of those aged 40-50.
Risk factors for adverse drug reactions
- Age.
- Polypharmacy.
- Female gender.
- Lower body weight.
- Hepatic or renal insufficiency.
- History of drug reactions.
Inappropriate Drugs
- Antibacterial to treat a viral infection.
- “Beers medications” – medications considered potentially inappropriate for older adults based on risk versus benefit (expert consensus).
You can follow science online on YouTube from this link: Science online
You can download Science Online application on Google Play from this link: Science online Apps on Google Play
Properties of cardiac muscles, Cardiac automaticity and Conduction of electrical impulses
Histology of the heart, Cardiomyocyte types, Ultrastructure and features of cardiac muscle fibers
Mediastinum contents, Aorta parts, Brachiocephalic trunk, Pulmonary trunk and Thoracic duct trunk
Electrocardiogram (ECG) importance, ECG test results, analysis and abnormalities
Heart & Pericardium structure, Abnormalities, and Development of the heart
Heart function, structure, Valves, Borders, Chambers and Surfaces
Cardiac Markers review, definition, list, test, and myoglobin function