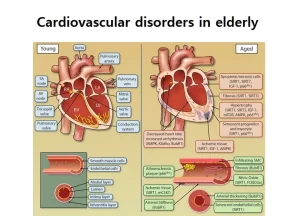
Cardiovascular disorders in elderly cause, symptoms, and Age-related cardiovascular changes
Cardiovascular disorders are a leading cause of illness and death among the elderly. Proper management, including lifestyle modifications, medication adherence, and regular medical checkups, can reduce the risk of complications and improve the quality of life for older adults.
Cardiovascular disorders in the elderly
Cardiovascular disorders are among the most common and serious health concerns affecting the elderly population. As people age, the cardiovascular system undergoes various changes that can increase the risk of developing these disorders.
Common Cardiovascular Disorders in the Elderly
Hypertension (High Blood Pressure)
- It is a chronic condition where the blood pressure in the arteries is persistently elevated.
- Causes: Age-related stiffening of the arteries, decreased kidney function, and lifestyle factors such as diet and lack of exercise.
- Symptoms: Often asymptomatic, but may cause headaches, dizziness, or blurred vision if severe.
- Hypertension increases the risk of heart disease, stroke, and kidney failure.
Coronary Artery Disease (CAD)
- It is caused by the buildup of plaque in the coronary arteries, leading to reduced blood flow to the heart.
- Causes: Atherosclerosis, high cholesterol, smoking, diabetes, and hypertension.
- Symptoms: Chest pain (angina), shortness of breath, and fatigue.
- Complications: Coronary Artery Disease can lead to heart attacks, heart failure, and arrhythmias.
Heart Failure
- Description: Heart failure occurs when the heart is unable to pump blood effectively, leading to a buildup of fluid in the lungs and other tissues.
- Causes: Previous heart attacks, hypertension, CAD, and diabetes.
- Symptoms are shortness of breath, fatigue, swelling in the legs, and difficulty exercising.
- Complications: Reduced quality of life, frequent hospitalizations, and increased mortality.
Atrial Fibrillation (AFib)
- Description: AFib is an irregular, often rapid heart rate that can lead to poor blood flow.
- Causes: Age-related changes in the heart, high blood pressure, heart disease, and thyroid problems.
- Symptoms: Palpitations, dizziness, weakness, and chest pain.
- Complications: Increases the risk of stroke and heart failure.
Valvular Heart Disease
- Description: This includes conditions that affect the heart valves, such as aortic stenosis and mitral regurgitation.
- Causes: Age-related degeneration of the valves, rheumatic fever, and infections.
- Symptoms: Fatigue, shortness of breath, and heart murmurs.
- Complications: Valvular Heart Disease can lead to heart failure and arrhythmias.
Peripheral Artery Disease (PAD)
- Description: PAD is a condition in which the arteries that supply blood to the limbs are narrowed or blocked.
- Causes: Atherosclerosis, smoking, diabetes, and high cholesterol.
- Symptoms: Leg pain when walking (claudication), numbness, and cold extremities.
- Complications: Increases the risk of heart attack, stroke, and limb amputation.
Causes and Risk Factors of Cardiovascular Disorders
- Natural aging processes contribute to the stiffening of arteries, reduced elasticity of blood vessels, and increased workload on the heart.
- Poor diet, lack of exercise, smoking, and excessive alcohol consumption.
- Diabetes, obesity, high cholesterol, and chronic kidney disease.
- A family history of cardiovascular disease can increase risk.
Symptoms of Cardiovascular Disorders
- Chest pain or discomfort.
- Shortness of breath.
- Palpitations or irregular heartbeats.
- Swelling in the legs or ankles.
- Dizziness or fainting.
- Fatigue and weakness.
- Cold or numb extremities.
Management and Treatment
- A healthy diet (low in salt, fat, and cholesterol), regular exercise, quitting smoking, and limiting alcohol intake.
- Antihypertensives, statins, anticoagulants, and medications to manage heart failure and arrhythmias.
- Blood pressure checks, cholesterol levels, and regular heart function tests.
- In some cases, angioplasty, stenting, valve replacement, or bypass surgery may be necessary.
- Educating elderly patients and their caregivers about the importance of adherence to medication, diet, and exercise regimens.
Age-related cardiovascular changes
Atrial fibrillation
Common arrhythmia is seen (in older individuals) and is often lone atrial fibrillation without a detectable underlying illness. This may be due to amyloidosis in the conducting system.
Sick sinus syndrome
- Deposition of collagen & lipid & amyloidosis→ Degeneration of pacemaker cell→ Tachy-brady cardia & atrioventricular block.
- Treated by: Replacement.
AV node
Calcification of the Aortic valve affects the AV node leading to slow conduction and complete heart block.
Ventricles
Amyloid deposition→ Restrictive cardiomyopathy & aging of myocardium → HF.
Diastolic changes
Left ventricular stiffness & amyloidosis → impaired diastolic filling which declines → 50% between ages 20 and 80 → diastolic heart failure (most common HP in elderly) Not diagnosed with ejection fraction, this type of heart failure is called Heart Failure with Preserved Ejection Fraction (HFpEF).
Systolic changes
The Aorta dilates and thickens due to calcification & atherosclerosis. → Increase afterload increase in SBP & wide pulse pressure. (systolic BP after age 30 years until the mid-70s, then through the 80s and 90s. (Isolated) systolic hypertension (most common in the elderly) Lt ventricular hypertrophy.
Coronaries
Atherosclerosis → MI, angina (80%) most common.
Decrease response to B Receptors
De Compensation during stress (no cop nor VC) → Narrow hemostatic capacity & postural hypotension. (most common type of hypotension & most common cause is antihypertensive drugs) 20% of old syncope.
Mitral & Aortic valves
- Thicken and stiffen → (calc/amyloidosis/atheroma) → stenosis → Flow murmur.
- The most common type of murmur is calcific aortic stenosis.
- Treatment: Surgical intervention, valve replacement or balloon dilatation or catheter dilatation atherosclerotic is a silent process.
- all stages are asymptomatic except the last stage which is called rupture pluck.
Coronary artery disease (CAD)
The incidence of CAD increases with age. Over 50% of all coronary events and 85% of all deaths from coronary artery disease occur after the age of 65.
Risk Factors
Traditional risk Factors
- Hypertension.
- Diabetes.
- Lack of exercise.
- The ratio of high total cholesterol to high-density lipoprotein.
- Smoking.
- Age.
Newer Risk Factors
- C-reactive protein
- Lipoprotein A
- Homocysteine
- Microalbuminuria.
How can subclinical cardiovascular disease be measured?
- Several measures have been developed to determine subclinical atherosclerotic disease:
- Electron-beam computerized tomography measures the amount of calcification in the coronary arteries.
- Carotid ultrasound can measure the degree of plaque in the carotid arteries to predict the risk of stroke.
- Ankle-brachial index (ABI) (the normal ratio is > 0.9 0.95).
You can subscribe to Science Online on YouTube from this link: Science Online
You can download Science online application on Google Play from this link: Science online Apps on Google Play
Cardiovascular system, Blood pressure regulation, Heart rate and its regulation
Factors affecting cardiac output, Stroke volume, Heart rate and blood pressure
Cardiac cycle importance, phases, diastole and systole, Aortic pulse curve and jugular venous
Electrocardiogram (ECG) importance, ECG test results, analysis and abnormalities
Heart & Pericardium structure, Abnormalities and Development of the heart