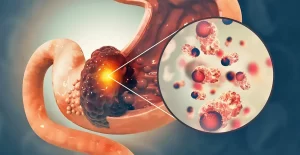
Stomach cancer causes, symptoms, treatment, and What is the survival rate of stomach cancer?
Stomach cancer is also known as gastric cancer, It occurs when abnormal cells grow and divide uncontrollably in the stomach. While it’s less common in Western countries, it’s a significant health concern globally. Early detection is crucial for successful treatment. Regular check-ups and being aware of symptoms can significantly improve outcomes.
Stomach cancer
Frequency of different types of gastric neoplasms
- Adenocarcinoma (90%).
- lymphoma (5%).
- Gastric Gastrointestinal stromal tumor (GIST 2%).
- Carcinoid (1%).
Gastric adenocarcinoma
Epidemiology
- Adenocarcinoma of the stomach is the second most common cancer Worldwide.
- It affects men more than women (2:1).
- The median age for gastric cancer in the United States is 70 years for males and 74 years for females.
Risk factors
- Diet (nitroso compounds, high salt, high in processed meat, and low fruits particularly citrus).
- Helicobacter pylori infection.
- Smoking.
- Pernicious anemia.
- Adenomatous polyps.
- Chronic atrophic gastritis.
- Prior radiation exposure or inherited syndromes.
Etiology and pathogenesis
Lauren classification (two separate forms):
- Intestinal: sporadic, H Pylori, high risk, and old patient (well differentiated).
- Diffuse: more aggressive than intestinal type, younger patients, associated with hereditary forms (undifferentiated).
Hereditary diffuse gastric cancer syndromes is caused by a germline mutation in CDH1 (encoding cadherin 1), critical for establishing intercellular d connections.
- The inheritance is autosomal dominant.
- Currently, prophylactic gastrectomy is recommended in afflicted individuals once they are >20 years of age.
Clinical features of cancer stomach
- Early asymptomatic in up to 80% of patients.
- Patients might present with dyspepsia.
- In advanced gastric cancer, weight loss (=60% of patients) and abdominal pain (=50%).
- Other symptoms include nausea, vomiting, anorexia, dysphagia, melena, and early satiety.
- Pyloric outlet obstruction in tumors of the antrum and pylorus.
- Tumors of the cardia can cause dysphagia (pseudo-achalasia)
- Rarely, paraneoplastic syndromes occur. Thrombophlebitis (Trousseau sign), neuropathies, nephrotic syndrome, DIC.
- Dermatologic paraneoplastic syndromes as (acanthosis nigricans) and pruritus (the sign of Leser- Trélat).
Signs
All physical signs are late events and include:
- Cachexia and signs of bowel obstruction are the most common abnormal findings.
- Occasionally, it is possible to detect an epigastric mass, hepatomegaly, ascites, and lower extremity edema.
- Succussion splash.
- Periumbilical metastasis (Sister Mary Joseph nodule).
- Enlarged lymph nodes: Virchow nodes (i.e., left supraclavicular) and Irish node (anterior axillary).
Diagnostic testing
Endoscopy
- The tumor appears as an exophytic polypoid mass or nodular mass.
- Take biopsies for histopathology diagnosis.
Laboratory investigations
- CBC: iron deficiency anemia.
- Tumor markers: carcino-embryonic antigen CEA, cancer antigen 19.9 (CA19.9) might be elevated.
Staging of the tumor
- Endoscopic ultrasound to assess the depth of penetration of the tumor in the wall, with FNA of suspected nodes for locoregional assessment.
- CT of chest and abdomen and PET scan for metastasis.
Treatment
Early-stage gastric cancer (Tis to T1a) (T1NOMO):
- Complete surgical resection: endoscopic mucosal resection is an alternative for Tis or T1a cancers at certain centers.
- No further treatment is necessary in absence of residual disease.
Locally advanced disease (T1b, T2, or higher, any N):
- Complete surgical resection (partial or total gastrectomy) if tumor is resectable, along with systemic therapy with or without radiation.
Metastatic disease (M1)
- Palliative chemotherapy or best supportive care (if unfit for treatment) and targeted therapy.
Primary gastric lymphoma (PGL)
- Accounts for 20% of all extra nodal lymphoma.
- Peak incidence between 50 and 60 years.
- Risk factors include H pylori infection, autoimmune disease, long-term immunosuppressives and celiac disease.
Histologic Subtypes
- Extranodal marginal zone B-cell lymphoma (MALT lymphoma): low-grade neoplasm, specific type of non-Hodgkin’s lymphoma, related to H pylori.
- Diffuse large B-cell lymphoma: A heterogeneous group of non-Hodgkin’s lymphoma; either occurs de novo or as a transformation from MALT lymphoma.
Clinical features
- Abdominal discomfort.
- Anorexia.
- Early satiety and weight loss.
- Gastric outlet obstruction.
- Maybe fever and night sweats.
Diagnosis
- Endoscopically: large, firm, rugal folds, eroded nodules, polypoid mass, and diffuse infiltration.
- H pylori testing and immunohistochemistry should be done in biopsies.
- Chest and abdomen CT scan to exclude systemic disease, lymph node extension, and/or to evaluate for infiltration of the adjacent structures.
- Gastric wall thickening or mass lesion can be identified in 85% of cases by imaging, while lymphadenopathy is reported in only 50%.
Ann Arbor staging of gastric lymphoma
- Stage I is confined to the stomach.
- Stage II involves lymph nodes within the abdomen.
- Stage III involvement on both sides of the diaphragm.
- Stage IV disseminated.
Treatment
HP-positive MALT lymphoma
- Antimicrobial therapy (PPI + amoxicillin + clarithromycin for 14 days) alone, if flat mucosal lesions in the stomach are present without lymph node involvement.
- Test for cure by urease breath test.
- Follow up by endoscopy after 3-6 months.
- Otherwise, systemic chemotherapy, radiotherapy, or surgery is done.
H pylori negative MALT lymphoma
- Antibiotics.
- Involved field irradiation.
- Systemic chemotherapy.
High-grade gastric lymphoma
- The treatment of PGL has shifted away from surgery and toward chemotherapy regimens. Today, Surgery is now limited to cases of perforation, hemorrhage, or obstruction due to the tumor.
- The most commonly used chemotherapeutic regimen for DLBCL of the stomach is a combination of cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP) and R-CHOP.
Gastrointestinal stromal tumor
- (GISTs) account for less than 1% of gastrointestinal (GI) tumors.
- The actual cell of origin of GISTs is a pluripotential mesenchymal stem cell programmed to differentiate into the interstitial cell of Cajal.
- These tumors express CD117 antigen (C-Kit), a gain of function mutation responsible for activating the growth of these tumors.
Endoscopically
- Submucosal lesions which most frequently grow endophytically or less common exophytic extraluminal.
- Size: (<1 cm to >40 cm in diameter).
- Site: Commonest site is in the stomach (50-70%).
Clinical picture
The most common symptoms are:
- Dyspepsia and rarely an abdominal mass is palpable.
- Symptoms are secondary to obstruction or hemorrhage.
- Manifestations of anemia.
Diagnosis
- Endoscopies define the lesion.
- EUS: FNA biopsy of tumor for tissue diagnosis.
- C.T. abdomen for metastasis.
Risk stratification
NIH classification system: It determined the risk of recurrence by categorizing patients into very low, low, intermediate, and high-risk groups by looking at the size and mitotic activity of the tumor.
High-risk GIST: Tumors > 5 cm in diameter plus a mitotic count higher than 5/50 high power fields (HpE) and tumors > 10 cm with any mitotic rate have a higher risk of recurrence, subsequently requiring adjuvant drug therapy (imatinib).
You can subscribe to Science Online on YouTube from this link: Science Online
You can download Science online application on Google Play from this link: Science online Apps on Google Play
Gastroesophageal reflux disease (GERD) cause, treatment, and How to treat eosinophilic esophagitis?
Pharynx function, anatomy, location, muscles, structure, and Esophagus parts
Tongue function, anatomy and structure, Types of lingual papillae and Types of cells in taste bud
Mouth Cavity divisions, anatomy, function, muscles, Contents of Soft palate and Hard palate
Temporal and infratemporal fossae contents, Muscles of mastication and Otic ganglion
Stomach parts, function, curvatures, orifices, peritoneal connections and Venous drainage of Stomach
Stomach Cancer (Gastric Adenocarcinoma) Symptoms, Causes and Treatment