Hepatic Encephalopathy diagnosis, cause, symptoms and treatment
Hepatic Encephalopathy is a brain dysfunction caused by liver insufficiency and/or (portosystemic shunts); it manifests as a wide spectrum of neurological or psychiatric abnormalities ranging from subclinical alterations to coma.
HE Burden of the disease
HE is the 2nd most common major complication in cirrhosis following ascites. Hospitalization is common and presents a burden on patients and the healthcare system with considerable cost, high morbidity, and mortality.
Pathogenesis of HE
Usually in a patient with hepatic, encephalopathy there are 3 important stations:
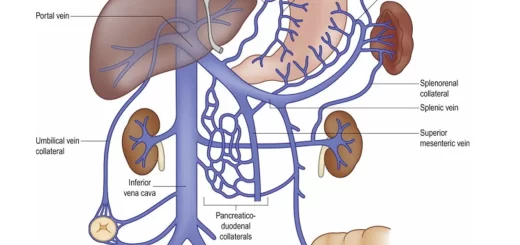
When the gut is overloaded by ammonia and nitrogenous overload toxic compounds, these toxic compounds pass into the portal blood to the liver or bypass the liver through the portosystemic shunts or pass through the compromised liver which cannot detoxicate all the amount of ammonia or toxic substances therefore, these toxic substances primarily the ammonia will pass into the systemic circulation and to the brain to induce the manifestations of HE.
The precipitating factors of HE
- Hypovolemia; diuretics, paracentesis (especially if there’s no volume replacement).
- Hyponatremia and electrolyte imbalance.
- Sepsis (from any infection elsewhere and in patients with cirrhosis sepsis or infection commonly come from SBP, cholangitis and/or UTI).
- Drugs (if they’re hepatotoxic leading to decompensation of the liver and other drugs which may affect the brain like benzodiazepine or opioids).
- High protein diet (will be associated with nitrogenous overload and high ammonia burden).
- GIT bleeding.
- Constipation.
- Concomitant disorder (anemia, alcohol intake).
- Manganese, systemic inflammatory response, oxidative stress, Sarcopenia, and Gut microbiota.
No single entity is responsible for HE, but rather it is a synergistic effect of multiple mechanisms, In this chart, excess ammonia in the systemic circulation should be consumed by the skeletal muscles of the patient, therefore it’s very important for a patient with liver cirrhosis to have a good skeletal muscle bulk.
Most of the patients are malnourished so we must encourage the patients for proper nutrition and for proper amount of protein to build up their muscles to consume this amount of ammonia, because if this amount of ammonia is excess in the systemic circulation it’ll pass to the brain.
Ammonia also may come from the kidney because one of the organs which is responsible for the secretion of ammonia is the kidney, so if you have a compromised kidney in a patient with chronic liver disease, it will share in the pathogenesis of nitrogenous overload, ammonia and hepatic encephalopathy, In the brain, the key cell which is responsible for the pathogenesis of the disease is astrocytes.
When ammonia passes from the blood vessels to the astrocytes, glutamic acid will be transformed into glutamine by the Glutamine synthetase enzyme. Astrocytes will absorb the surrounding water and it’ll be edematous and swollen. This swollen astrocyte will be responsible for the manifestations of the disease.
Clinical manifestations
Neurologic and psychiatric manifestations
Alterations in intellectual capacity, memory, emotional, behavioral, psychomotor speed, and fine motor skills, These can lead to apathy, irritability, decreased energy level, impaired sleep-wake cycle, impaired cognition, diminished consciousness, asterixis or loss of motor control, Disorientation and/or asterixis are the beginning of overt HE (grade 2-4).
Asterixis means that the patient can’t maintain the posture of his hands in a dorsiflexion pattern and tremors start to appear. Asterixis is one of the diagnostic findings of HE and it differentiates between cover and overt encephalopathy. the most important classification and clinical criteria for a patient with HE is West Haven criteria which defines and classifies HE into 2 main stages:
- Covert: the disease is not clinically manifest. It has minimal and grade 1.
- Overt: the disease is clinically manifest. It has grades 2, 3, and 4.
HE has been classified according to:
- Severity of manifestations (West Haven) (classifies the patient from very mild symptoms up to stupor and even coma).
- Time course (Episodic, Recurrent, Persistent).
- Underlying disease (Type A, B, C).
Grading of hepatic encephalopathy (West Haven)
- Stage 0: State of consciousness: No change in personality or behaviour, No asterixis (flapping tremor).
- Stage 1: State of consciousness: Impaired concentration and attention span, Sleep disturbance, slurred speech, Euphoria or depression. Asterixis present.
- Stage 2: State of consciousness: Lethargy, drowsiness, apathy or aggression Disorientation, inappropriate behaviour, slurred speech.
- Stage 3: State of consciousness: Confusion and disorientation, bizarre behaviour, Drowsiness or stupor, Asterixis usually absent.
- Stage 4: State of consciousness: Comatose with no response to voice commands, Minimal or absent response to painful stimuli 4.
You can subscribe to science online on YouTube from this link: Science Online
You can download Science Online application on Google Play from this link: Science Online Apps on Google Play
Spontaneous bacterial peritonitis symptoms, diagnosis, treatment, causes and antibiotics
Hepatorenal syndrome (HRS) risk factors, diagnosis, symptoms, types, causes and treatment
Refractory ascites symptoms, cause, types and treatment of refractory ascites in cirrhosis
Ascites cause, grades, symptoms, diagnosis and Treatment of cirrhotic ascites
Liver Cirrhosis causes, symptoms, treatment & stages, Liver Biopsy and treatment of PHTN
Viral hepatitis, HDV symptoms, Treatment of acute HCV, Occult hepatitis C and HEV
Acute Hepatitis Causes, Diagnosis, and Treatment, Chronic hepatitis and Liver biopsy
Liver development, congenital anomalies, function & Pancreas development