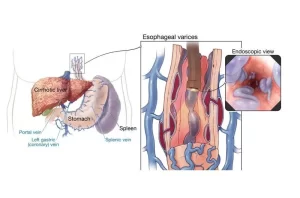
Gastro-esophageal varices cause, treatment, and therapy of variceal bleeding
The transition levels must be prevented (prevent the formation or growth or bleeding or treat acute bleeding and prevent rebleeding), All cirrhotic patients should be screened for varices at diagnosis. EGD (Esophagogastroduodenoscopy) will show large esophageal varices with a red color sign (tend to bleed) or portal hypertensive gastropathy.
Gastro-esophageal varices
By endoscope it is called mosaic appearance or snakeskin appearance, The diagnosis of PHG is made endoscopically.
Natural Hx of Esophageal varices = increases portal pressure >10 → Formation→ dilation→rupture >12 mmHg.
Prophylaxis of variceal bleeding
1. Cirrhosis, no varices
- No specific pre-primary prophylaxis.
- Treat underlying liver disease.
- f/u (follow-up) endoscopy after years.
2. Primary Prophylaxis of Variceal bleeding
- There is no indication to treat patients of PHTN without varices.
- Patients with small varices could be treated, especially if there are red color signs and/or if the patient is in Child C class.
- Patients with large varices with risk signs of bleeding are treated by band ligation.
- Beta-blockers should be the treatment of choice.
- Offering EBL to those patients with moderate or large varices and contraindications or intolerance to Beta-blockers.
3. Secondary prophylaxis of Variceal Rebleeding
A. Pharmacological: B Blockers
- Non-selective beta-blockers are effective in preventing variceal rebleeding.
- Adding isosorbide-5-mononitrate (IsMn) enhances the HVPG reduction caused by non-selective beta-blockers.
B. Endoscopic: Repeated sessions of band ligation
- EBL is more effective than sclerotherapy in preventing rebleeding, with less side effects and requires a lower number of sessions.
C. Radiological: TIPS (interventional radiology)
D. Surgical: If the degree of cirrhosis is Child-Pugh class A or B (Shunt operation is used).
Treatment of Acute Variceal Bleeding
General management
- Careful replacement of volemia: keep Hb between 7 and 9 g/dl.
- One of the main complications associated with variceal hemorrhage is a bacterial infection.
- Short-term antibiotic prophylaxis decreases the rate of infection & increases survival and is the standard of care.
- Although norfloxacin (Quinolones) has been recommended by consensus opinion, a recent RCT suggests that I.V ceftriaxone (3rd generation cephalosporin) may be a superior option in patients with advanced liver disease and hemodynamic instability.
Early drug treatment
- B Blockers are not useful or rapid in the acute stage.
- Vasoconstrictors are available (somatostatin, terlipressin, vapreotide), but octreotide is the only one that is approved by the US Food and Drug Administration (FDA).
- In Europe and Egypt. Terlipressin is more used.
- The favorable safety profile of this agent allows initiation of treatment before diagnostic endoscopy that is, at the time the diagnosis is suspected in the emergency department- and treatment can be continued for the next 2-5 days after EBL.
Pharmacological therapy of variceal bleeding
- Vasopressin.
- Vasopressin+Nitroglycerin
- Terlipressin
- Somatostatin and analogues (octreotide), the last 2 choices are the best (70 % efficacy to arrest bleeding).
In acute variceal hemorrhage, pharmacologic therapy (specifically splanchnic vasoconstrictors) in combination with endoscopic therapy have been found to be more effective in controlling bleeding than either treatment alone. However, the addition of pharmacologic therapy to endoscopy did not appear to significantly reduce mortality, General management + drug Rx followed by Endoscopic therapy if failed → 2nd course of Endoscopic Rx-if failed or rebleed- TIPS
Endoscopic therapy
A. Esophageal varices sclerotherapy
- Blue: Large varix with red color sign in a lower esophagus.
- Red: Injection sclerotherapy using sclerosant with contrast medium. Thus in turn will lead to fibrosis to varices to stop bleeding.
- Green: Ulcers/erosions/ adhesions are very common post-sclerotherapy.
B. Endoscopic Variceal Band Ligation
- It Should be performed in the 1st 12 hours, (preferably 1st 6 hrs), after stabilizing the patient. (It is preferred more than sclerotherapy). The bleeding stopped at 90% & Rebleeding rate was 15-20%.
- Compared with sclerotherapy: Less rebleeding & mortality, Fewer complications, and Fewer treatment sessions.
- Balloon tamponade must be used in massive bleeding as a temporary “bridge” until definitive treatment, Expandable stents: a new alternative to balloons with no major complications.
Trans-jugular intrahepatic portosystemic shunting (TIPS)
It connects the portal and systemic circulation to transmit high portal pressure into the systemic circulation to stop bleeding. It is still considered to be a salvage therapy in the control of acute hemorrhage. Early TIPS placement (within 24 hours of hemorrhage) was associated with significantly improved survival in high-risk patients (i.e., those with an HVPG > 20 mm Hg) and may play an earlier role in the treatment of acute variceal hemorrhage. but it is expensive.
Gastric Varices
- Present in 5-30% of patients with cirrhosis.
- Account for 10-15% of variceal bleeding episodes.
- Risk factors: size, Child class, presence of red spots. Standard endoscopic therapy: Cyanoacrylate.
Cyanoacrylate: Compared to endoscopic injection sclerotherapy (EIS) or esophageal variceal ligation (EVL), endoscopic variceal obturation with a tissue adhesive such as N-butyl cyanoacrylate, or isobutyl-2-cyanoacrylate is more effective for acute fundic gastric variceal bleeding.
In patients who have contraindications or intolerance to beta-blockers, (band ligation is the preferred treatment. In patients who fail endoscopic and pharmacologic treatment, TIPS or surgical shunts are effective for Child A-B patients. Transplantation provides good long-term outcomes in Child B-C cirrhosis.
You can subscribe to science online on YouTube from this link: Science Online
You can download Science Online application on Google Play from this link: Science Online Apps on Google Play
Liver Cirrhosis causes, symptoms, treatment & stages, Liver Biopsy and treatment of PHTN
Viral hepatitis, HDV symptoms, Treatment of acute HCV, Occult hepatitis C and HEV
Acute Hepatitis Causes, Diagnosis, and Treatment, Chronic hepatitis and Liver biopsy
Portal Venous System, Histological structure of Liver, portal vein and its tributaries
Liver development, congenital anomalies, function & Pancreas development