Peptic Ulcer Diseases symptoms, treatment, What causes ulcers besides H. pylori?
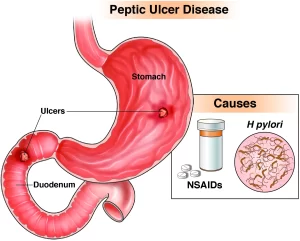
Peptic ulcer disease is characterized by open sores that develop in the lining of the stomach or duodenum (the first part of the small intestine). These sores, known as ulcers, can cause significant discomfort and complications if left untreated.
Peptic Ulcer Disease (PUD)
- Responsible for 10% of medical costs for digestive diseases.
- Natural history: Resolution, Complications: Bleeding, perforation, obstruction.
- The patient’s ulcer history predicts future behavior.
- Those with a history of complications have an increased risk of future complications.
- Ulcers refractory to initial healing are likely to rapidly recur, and ulcers that have recurred are likely to continue to do so.
- Long duration of symptoms before presentation is more likely associated with poor response to therapy.
Symptoms of Peptic Ulcer Disease
- Burning or gnawing stomach pain.
- Heartburn.
- Indigestion.
- Nausea.
- Vomiting.
- Loss of appetite.
- Weight loss (in severe cases).
- Blood in vomit (dark, coffee-ground appearance).
- Black or tarry stools.
Causes of diseases associated with peptic ulcer:
- Most common: Helicobacter pylori infection, and NSAIDS.
- Unusual:
- Physiologic stress in ICU setting.
- Herpes simplex virus type 1 infection.
- Gastrinoma (Zollinger-Ellison syndrome).
- Carcinoid syndrome.
- Corticosteroids (a risk factor when added to NSAIDs).
- Basophilia in myeloproliferative disorders.
- Systemic mastocytosis.
- Cytomegalovirus infection.
- Antral G cell hyperfunction.
- Helicobacter heilmanni infection.
- Idiopathic hypersecretory (H. pylori-ve) duodenal ulcer.
- Radiation.
- Duodenal obstruction (eg. Annular Pancreas).
- Chemotherapy (eg. Hepatic infusion of 5-fluorouracil).
- Sarcoidosis.
- Idiopathic.
- Drug-induced ulcers (eg. Potassium chloride, bisphosphonates, mycophenolate mofetil).
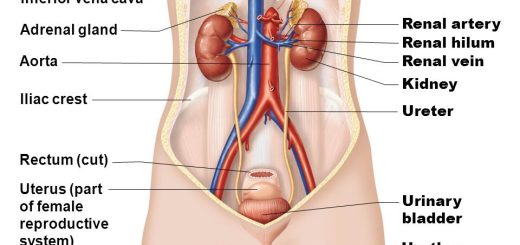
Diseases associated with peptic ulcer
- Chronic obstructive pulmonary disease.
- Cirrhosis.
- Renal failure.
- Organ transplantation.
- Rheumatic disease (via the use of NSAIDs).
Helicobacter pylori
It is about 3 μm long and 0.5 μm in diameter, microaerophilic (requires oxygen), neutralophilic (adapting to highly acidic environment), helix-shaped (curved rod), gram-negative bacteria colonizing upper gastrointestinal tract.
H. pylori is contagious, where the person-to-person transmission is either by the fecal-oral or oral-oral route. H. pylori infection and pathogenicity are well connected and coordinated by different mechanisms to adapt to the acidic environment in the stomach; to attack the stomach wall by weakening the gastric mucosal barrier using different molecules to adhere the host stomach lining: protecting itself from oxidative stress; inducing gastritis or inflammation, formation of ulcers, and inducing gastric cancer.
It can cause:
- Gastritis.
- PUD (peptic ulcer disease).
- Gastric CA.
- MALT Lymphoma.
- Functional Dyspepsia.
- GERD.
Gastric acid secretion and H. pylori
Stimulated acid output is increased in patients with H-pylori infections, whether they have duodenal ulcers with the infection or not. However, patients with duodenal ulcers were noticed to have a higher increase in acid output than healthy individuals.
Possible mechanisms of Ulcerogenesis in H. pylori
When bacteria colonize the stomach inflammation induces G cells of the antrum. G cells secrete the hormone gastrin, which travels to the parietal cells of the fundus via the bloodstream. Gastrin stimulates the secretion of acid from the parietal cells and increases the number of parietal cells. The increased load of acid damages epithelial cells of the duodenum resulting in ulcers.
Extra digestive manifestations of H. pylori
- Vascular: IHD (ischemic heart disease) Raynaud’s phenomenon, headache, and migraine.
- Autoimmune: Henoch-Schoenlein purpura, Sjogren’s syndrome, ITP.
- Others: Rosacea and urticaria, sideropenic anemia, growth retardation, amenorrhea and late menarche, halitosis, extra gastric MALT lymphoma, and NIDDM (non-insulin-dependent diabetes mellitus).
Diagnosis of H. pylori
Endoscopy-based invasive tests:
- Rapid urease test.
- Direct microscopy.
- Histology.
- Culture.
- DNA probes/PCR.
Non-invasive tests:
- 13/14C-urea breath test (UBT).
- Serology (IgG, IgM).
- PCR in saliva and feces.
- Stool H-Pylori antigen.
What diagnostic test should I depend on?
Screening for “latent” infection:
- Serology: Quick, inexpensive, reliable.
- Could be a scar from a past infection and doesn’t reflect status.
- Positive serology should be confirmed by UBT or stool Ag.
- Treat only on positive confirmed results.
During endoscopy:
- Take 2 mucosal samples.
- First: RUT (rapid urease test), if positive, start treatment.
- Second: histopathology
- Examine only when negative RUT.
- Treat only on positive results.
Consensus on treating of H. pylori (Strongly recommended):
- PUD.
- Gastric lymphoma.
- Atrophic gastritis.
- Patients with gastric carcinoma (post-resection).
- Close relatives of gastric CA patients.
Treatment options:
- Antibiotics (Clarithromycin, Amoxycillin, Metronidazole, Tetracycline, Furazolidone).
- Adjuvant drugs (PPI, RBC).
Protocols of H. pylori eradication
- Monotherapy
- Dual therapy: 1 A.B+1 Adjuvant.
- Triple therapy: 2 A.B+ 1 Adjuvant.
- Quadruple therapy: 2 A.B + 2 Adjuvant.
First line therapy
PPI Options
- Omeprazole 20 mg twice daily.
- Lanzoprazole 30 mg twice daily.
- Pantoprazole 40 mg twice daily.
- Rabeprazole 20 mg twice daily.
- Esomeprazole 40 mg twice daily.
PPI Based Triple Therapy
PPI Bid + Clarithromycin 500 mg Bid + Amoxicillin 1000 mg Bid OR Metronidazole 500 mg Bid.
Second line therapy
- Quadruple therapy: 67-88% Success.
- Rifabutin-based therapy (PPI + Amoxicillin + Rifabutin): 72% success.
- Consecutive therapies: 100% success.
Quadruple therapy
PPI Bid + Bismuth 2 Tabs qid + Metronidazole 250 tid + Tetracycline 500 mg qid for 10-14 days.
Duration of eradication therapy
Regimens of very short duration (<7 days)
- European guidelines: at least 7 days.
- Few reports of success of as short as 3-4 days treatment but usually with 3 A.B.
Regimens with duration (>7 days)
- American guidelines: At least 10-14 days.
- 10-14 days better in high bacterial load.
- 10=14 days, but better than 7 days
Follow-up after therapy
- Recurrence of symptoms.
- Endoscopy is required: RUT, histo-biopsy.
- Endoscopy is not required: UBT, stool antigen.
Why not serology?
- 23 H. pylori volunteers were Confirmed by biopsy. Eradication was confirmed by biopsy. Serology was obtained monthly for 18 months.
- At 3 months, a 50% decrease in Ab titer was noticed.
- At 18 months, 60% of patients had undetectable Abs.
A serology after treatment should be done at least ONE YEAR after eradication.
- Check only after > 4 weeks.
- Cure = No organism > 4 weeks after cessation of anti-microbial treatment.
Options after the failure of Eradication
- Antibody susceptibility available gives antibodies.
- Antibody susceptibility is not available: give metro-clarithromycin.
Smoking
- Adverse effects on mucosal aggressive and protective factors.
- Studies in pre-H. pylori era found that smoking had a facilitative role for PUD.
- Smokers are more likely to develop ulcers. Ulcers were more difficult to treat with higher rates of recurrence.
NSAIDs
- It is the major reason for peptic ulcers not caused by H. pylori.
- Associated with increased risk of complications.
- The odds ratio for GU = 5.9 and DU = 4.9.
- The odds ratio for hemorrhage was 5.2, as was for perforation.
- They are responsible for a significant number of PU refractory therapy.
- 40% of patients may not report using NSAIDs.
- Patients with a peptic ulcer who must continue NSAIDs should be maintained on either PPUl or H2RA.
- COX-2 selective NSAIDs offer a good alternative.
GIT lesions induced by NSAIDs
- Acute mucosal lesions: Petechia, erosions, acute ulcers.
- Chronic/deep GD ulcers.
- Complications: Gl bleeding, Perforation, Obstruction.
Age and sex
- Onset of ulcer disease in youth and positive family history may be associated with poor healing.
- Ulcers in older patients may heal more slowly.
- Older patients are more likely to bleed, rebleed, require more transfusions, and have prolonged hospital stays.
Alcohol
- Modest alcohol consumption doesn’t appear to retard the cure of PU.
- Alcohol abuse interferes with ulcer healing.
Diet
- Frequent feedings cause less gastric distension which may lead to sustained stimulation of acid secretion.
- Milk was a main therapy for PU because of its soothing nature, until it was shown to be a strong acid secretagogue because of its calcium and protein content.
- Milk use should not be discouraged in patients who find these measures beneficial.
- Patients should be told that milk is not a therapy for ulcers.
Clinical picture of PU
- Uncomplicated.
- Complicated: Bleeding, Perforation, Obstruction.
Uncomplicated
Nausea, Anorexia, Dyspepsia, Abdominal pain, Vomiting, Loss of weight.
Complicated
- Bleeding: hematemesis (coffee ground), melena, occult positive anemia, hematochezia (rare).
- Obstruction: vomiting of large amounts and post-prandial > 12 hours, succussion splash.
- Perforation: severe abdominal pain, hypotension/shock, rigidity, rebound tenderness, air under diaphragm.
Diagnosis
Barium meal
- Diagnose ulcer: Ulcer niche.
- Diagnose complications: Obstruction, perforation.
- Contraindicated during bleeding.
- Can’t diagnose healing of ulcer.
Plain X-ray
Air under diaphragm = perforation.
Endoscopy
- Diagnose ulcer.
- Biopsies for H.P. or Malignancy.
- Diagnose complications: Bleeding, obstruction.
- Contraindicated in perforation.
- Treatment of bleeding ulcer.
- Treatment of obstructing ulcer.
Treatment of PU
- H. pylori-positive uncomplicated ulcer.
- H. pylori unrelated uncomplicated ulcer.
Drugs used in the treatment of PU
H2 RA, PPI, prostaglandins, anti-H. pylori therapy.
ACG Recommendations of PPl in Treatment of Acid-related Disorders
Active and maintenance therapy of gastro-duodenal ulcers:
- Omeprazole 20 mg.
- Lanzoprazole 30 mg.
- Pantoprazole 40 mg.
- Rabeprazole 20 mg.
- Esomeprazole 40 mg.
Prevention of NSAID-induced ulcers:
All PPIs above, As a rule, PUs treated for 4 weeks and GU for 8 weeks.
Causes of refractory or recurrent PU
- Persisting HP infection: poor compliance, resistant organism, inadequate HP regimen.
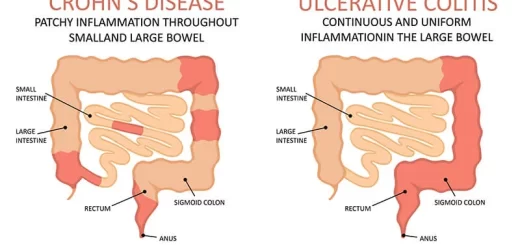
- Persisting or recurrent ulcer, no HP: false negative HP testing, continued or undiscovered NSAIDs use, delayed healing (dense fibrosis, heavy smoking, giant ulcer), inadequate inhibition of acid secretion (H2 receptor antagonist tolerance or PPI resistance), hypersecretory states (gastrinoma, antral G cell hyperfunction, idiopathic hypersecretory duodenal ulcer), uncommon forms of peptic ulcer, non-peptic ulcer (cancer, Crohn’s disease other infections).
- Persisting symptoms, no ulcer: another diagnosis.
Treatment of Bleeding ulcer
- Hemodynamic Resuscitation.
- Anti-Helicobacter therapy.
- Endoscopic methods: Heater Probe, Coagulation, Sclerotherapy, Band Ligation, APC, Laser therapy.
Treatment of Obstruction
- Resuscitation.
- NG suction of gastric contents.
- Endoscopic Balloon Dilatation.
- Surgical By-pass.
Treatment of Perforation
- Resuscitation.
- NPO.
- IV fluids.
- IVA.B.
- Immediate surgical closure (most important).
- Endoscopic clips (when noticed during endoscopy small, recent).
You can subscribe to Science Online on YouTube from this link: Science Online
You can download Science online application on Google Play from this link: Science online Apps on Google Play
Gastroesophageal reflux disease (GERD) cause, treatment and How to treat eosinophilic esophagitis?
Pharynx function, anatomy, location, muscles, structure, and Esophagus parts
Tongue function, anatomy and structure, Types of lingual papillae and Types of cells in taste bud
Mouth Cavity divisions, anatomy, function, muscles, Contents of Soft palate and Hard palate
Temporal and infratemporal fossae contents, Muscles of mastication and Otic ganglion
Stomach parts, function, curvatures, orifices, peritoneal connections and Venous drainage of Stomach