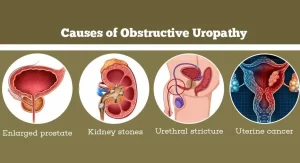
Obstructive Uropathy, What are the causes of urinary tract obstruction? and How do you fix uropathy?
Obstructive uropathy occurs when the flow of urine is blocked somewhere in the urinary tract. This blockage can cause urine to back up and damage the kidneys. There are many different causes of obstructive uropathy, including Kidney stones, Blood clots, Tumors Strictures (narrowing) of the urinary tract, Enlarged prostate gland (in men), and Abnormal valves in the urethra (in infants).
Obstructive Uropathy
Pathological changes in the urinary tract that result from obstruction to the flow of urine. The obstructive lesion is either infravesical (at the level of the urethra or bladder neck) or supravesical (at the level of the ureter, renal pelvis, or neck of a calyx). Supravesical obstruction will present by hydronephrosis while infravesical obstruction will present by retention which may be acute, chronic, or acute on top of chronic retention.
Hydronephrosis
Chronic progressive aseptic dilatation of the pelvicalyceal system due to complete intermittent or partial obstruction with secondary ischemic pressure atrophy of the renal parenchyma.
Causes
A. Nonobstructive causes: reflux and megaureter.
B. Obstructive causes: due to partial or intermittent complete obstruction
I. Upper urinary obstruction (kidney or ureter)
- Inside the lumen e.g. stone.
- In the wall e.g. stricture, tumor, ureterocele, pelviureteric junction obstruction.
- Pressure from outside e.g. aberrant renal vessels, gravid uterus, retroperitoneal fibrosis, lymphadenopathy.
II. Lower urinary obstruction: causing bilateral hydronephrosis
- Vesical e.g. bladder neck obstruction, contracted bladder.
- Urethral eg. congenital valves, stricture, or prostatic enlargement.
Symptoms and signs
- There are no symptoms and the condition is discovered accidentally.
- Pain is either in the form of mild aching pain in the loin due to distension of the renal capsule or renal colic if a stone is the cause of obstruction.
- A swelling in the loin occuring in advanced cases. It has the characteristics of a renal swelling, tense cystic, and is not tender unless hydronephrosis is infected, with a bossy surface.
- Gastrointestinal symptoms as nausea and vomiting.
- Symptoms and signs of uremia in bilateral advanced hydronephrosis.
- Symptoms and signs of the obstructing cause e.g. enlarged prostate or bladder carcinoma.
Diagnosis
a) Unilateral or bilateral.
b) Degree of hydronephrosis.
c) Cause of hydronephrosis.
1. Symptoms: of hydronephrosis and its cause.
2. Physical examination:
- General examination may show signs of renal failure in advanced bilateral hydronephrosis.
- Abdominal examination may reveal cystic renal swelling in the loin in advanced cases.
- Digital rectal examination may discover a lower urinary tract obstruction as prostatic enlargement.
3. X-ray findings: may detect urinary stones.
4. Intravenous urography:
- Establishes the degree and functional capacity of the hydronephrotic kidney.
- Proves the normality of the other kidney in unilateral hydronephrosis.
- May reveal the cause of obstruction e.g. stricture ureter and radiolucent stone.
5. Ultrasound: shows dilatation of the pelvicalyceal system and degree of atrophy of the parenchyma.
6. CT with or without contrast to detect the level of obstruction and the cause of hydronephrosis.
7. MRU for neonates and children.
8. VCUG to diagnose reflux as a cause of hydronephrosis.
9. Renal function test: blood urea, serum creatinine, creatinine clearance tests.
Differential diagnosis
- Pyonephrosis and infected hydronephrosis: tender swelling, fever, malaise.
- Renal tumor: solid renal mass.
- Polycystic kidney (non-communicating cysts).
Treatment
Certain factors decide the choice of treatment for hydronephrosis:
- Whether unilateral or bilateral.
- Obstructive or non-obstructive.
- Degree and functional capacity of the hydronephrotic kidney.
- Chance of removal of the cause.
- Presence of complications especially infection.
Obstructive hydronephrosis
Unilateral hydronephrosis:
- In early cases, removal of the cause is required.
- In complicated cases, drainage of the kidney by nephrostomy insertion or DJ then reassessing the renal function and treating the cause.
- In advanced cases with nonfunctioning kidneys and good opposite kidneys, nephrectomy is indicated if symptomatic.
Bilateral hydronephrosis:
- In early cases, removal of the cause is required.
- In complicated cases, bladder drainage by urethral or suprapubic catheter if the cause is infravesical and insertion of bilateral nephrostomies or bilateral DJ if the bilateral ureteral obstruction is the cause, then reassessing the renal functions before treating the cause.
- In some cases, hemodialysis maybe indicated because of renal failure.
- In advanced cases, if the renal function is not restored, the patient will need permanent dialysis or renal transplantation.
Non-obstructive hydronephrosis:
Treatment of reflux or megaureter either unilateral or bilateral.
Retention of urine
A) Acute Urinary Retention
Definition: Sudden painful inability to pass urine perurethra in the presence of a full bladder.
Etiology:
Any lesion that obstructs the lumen of the bladder neck or urethra; e.g. impacted urethral stone, urethral injury, benign prostatic hyperplasia.
Treatment:
- The bladder is emptied as an emergency by urethral catheterization. If this is not possible, e.g. in the presence of urethral injury, suprapubic cystostomy is done.
- Bladder drainage is continued until the cause of acute retention is treated.
- Treatment of the cause.
B) Chronic Urinary Retention
Definition: It is the painless inability to evacuate the bladder completely.
Pathogenesis
With long standing chronic obstruction, the bladder will try to increase its contraction to overcome the distal chronic obstruction (BPH, urethral stricture) in order to evacuate the bladder completely.
With time the patient will micturite but will have a significant amount of residual urine > 100cc.
In the presence of high resistance caused by an obstructive lesion in the urethra or bladder neck, the detrusor muscle contractions become stronger to overcome the high resistance and to empty the bladder completely.
Continuous strong muscle contractions result in progressive hypertrophy of the detrusor muscle bundles. The hypertrophied muscle bundles protrude significantly beneath the covering bladder mucosa. They appear by cystoscopy as course wavy interlacing bundles, and are called trabecula (trabeculation of the detrusor).
Areas in the bladder wall between interlacing trabecula are covered by mucosa only, These areas represent weak points in the bladder wall. High intravesical pressure can cause herniation of the bladder mucosa at these weak points. A “cellule” is a small herniation within the bladder wall. A diverticulum is a bigger herniation that extends beyond the bladder wall.
Detrusor muscle will eventually get fatigued from sustained strong contractions against high resistance. Later the bladder will be decompensated and the patient will be unable to evacuate the bladder.
With incomplete bladder emptying in a decompensated bladder, the volume of residual urine increases progressively, In an advanced stage, the volume of residual urine becomes equal to the bladder capacity, At this stage, urine entering the full bladder from the ureters escapes involuntarily through the urethra: “overflow incontinence”.
High volumes of residual urine will hinder urine flow from the ureters to the bladder causing bilateral hydroureters and bilateral hydronephrosis. If neglected, renal failure and uremia occur.
Types
- Chronic retention with residual urine. The patient will have a desire to micturate and will have a normal act of micturition BUT with significant residual urine. It might be associated with nocturnal enuresis in adults.
- Chronic retention with overflow incontinence: the patient will have no desire to micturate, full bladder, and total incontinence.
Causes
1. Neurogenic:
- Spinal injury.
- Multiple sclerosis.
- Polyneuropathy as in DM.
2. Drugs: anticholinergics, antihistaminics, drugs for irritable bowel syndrome.
3. Urinary causes:
- Long standing fibrous prostate (BPH) or neglected treatment of BPH.
- Sphincteric dyssynergia.
- Urethral stricture.
- Cystocele, uterine polyp, rectocele.
Complaints
- Frequency: the presence of residual urine due to incomplete bladder emptying will decrease the bladder capacity and will lead to an increased number of micturitions.
- Obstructive urinary symptoms in early stages of chronic retention.
- Urinary incontinence (overflow incontinence) or nocturnal enuresis.
- Symptoms of complications: recurrent UTI, hematuria secondary to bladder stones, and renal insufficiency.
Diagnosis
1. History of the cause: e.g. BPH, urethral stricture, neurogenic cause.
2. Examination: Suprapubic bulge due to the presence of a full bladder.
3. Laboratory investigations:
- Urine analysis: pus cells and red blood cells.
- Renal functions: blood urea and serum creatinine (usually elevated).
4. Radiology:
Post voiding US will show high residual urine volume or even full bladder in late stages. The US of the bladder may show bladder diverticula.
5. Urodynamic study for neurogenic bladder.
6. Cystoscopy: shows bladder trabecula and diverticula.
Treatment
Bladder drainage with an indwelling urethral or suprapubic catheter. The drained bladder eases the flow of urine from the kidneys, and uremia will be reversed, then treatment of the cause e.g. TURP for BPH, endoscopic visual urethrotomy for urethral stricture.
C) Acute on top of chronic retention
Definition: Acute inability to pass urine in a patient with chronic urinary retention.
Pathogenesis
- Patients with chronic urinary retention and overflow incontinence may be complicated by bladder stone formation or may have an enlarged obstructing prostate that will obstruct the urine outflow.
- It is an emergency condition and is usually associated with renal insufficiency or renal failure.
Treatment
- Emergency intervention to treat uremia. According to the laboratory investigations, the patient may need hemodialysis or urinary catheterization, or urinary diversion by insertion of bilateral PCN.
- Treatment of the cause.
You can subscribe to Science Online on YouTube from this link: Science Online
You can download Science Online application on Google Play from this link: Science Online Apps on Google Play
Urolithiasis, Stones in the kidney or ureter, How do you treat urolithiasis?
Anomalies of the bladder and urethra, Urinary tract abnormalities symptoms
What are urinary tract infections?, kidney problems, Urinary retention and Bladder stones
Functions of Kidneys, Role of Kidney in glucose homeostasis, Lipid & protein metabolism
Histological structure of kidneys, Uriniferous tubules and Types of nephrons
Urine formation, Factors affecting Glomerular filtration rate, Tubular reabsorption and secretion
Urinary passages function, structure of Ureter, Urinary bladder & Uvulae vesicae
Urinary system structure, function, anatomy, organs, Blood supply and Importance of renal fascia
Urinary bladder structure, function, Control of micturition by Brain & Voluntary micturition