Nutrition assessment and falls in elderly, Malnutrition Risk and Falls among Community
Addressing nutritional deficiencies and ensuring proper intake of essential nutrients are key components of fall prevention in the elderly. By assessing their nutritional status and addressing areas of deficiency, healthcare providers can reduce the risk of falls, improve overall quality of life, and promote independence in older adults.
Nutrition assessment and falls in elderly
Nutrition assessment and falls in the elderly are closely related, as nutritional status can impact physical health, strength, balance, and overall fall risk.
1. Nutritional Factors Affecting Fall Risk
- Protein Deficiency: Insufficient protein intake can lead to muscle weakness and sarcopenia (loss of muscle mass), both of which reduce balance and mobility, increasing the risk of falls.
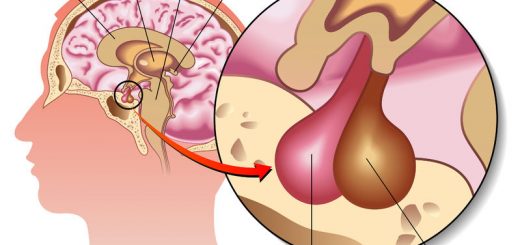
- Vitamin D is necessary for bone health and muscle function, Low levels can lead to weakened bones (osteoporosis) and impaired muscle performance, making falls more likely. A lack of Vitamin D is also associated with poor balance and an increased likelihood of fractures if a fall occurs.
- Calcium is essential for maintaining strong bones, A deficiency can lead to osteoporosis, increasing the risk of bone fractures from falls.
- Dehydration: Older adults are at higher risk for dehydration, which can lead to dizziness, confusion, and muscle cramps, all of which increase the likelihood of falling.
- Low Body Weight and Malnutrition: Elderly people who are underweight or malnourished may experience general weakness, loss of muscle mass, and poor endurance, contributing to instability and higher fall risk.
- Overweight or Obesity: Being overweight can also affect balance and mobility, and excess body weight can lead to joint pain (such as arthritis), further increasing fall risk.
2. Comprehensive Nutrition Assessment
- Dietary Intake: Assess the adequacy of calories, proteins, vitamins, and minerals in the diet. This includes looking at the consumption of nutrient-rich foods such as fruits, vegetables, lean proteins, and whole grains.
- Anthropometric Measurements: Weight, height, body mass index (BMI), and muscle mass can be measured to assess overall nutritional health. A decline in weight without trying, or low BMI, could indicate malnutrition.
- Biochemical Markers: Blood tests can reveal deficiencies in key nutrients like Vitamin D, Calcium, and electrolytes that affect bone and muscle health. They may also indicate anemia (iron or vitamin B12 deficiency), which could affect energy levels and mobility.
- Physical Functioning: Muscle strength, grip strength, gait speed, and balance tests help assess physical frailty, which may indicate poor nutrition. Reduced muscle mass (sarcopenia) and functional decline are often related to inadequate nutrition and predict fall risk.
- Medications and Chronic Conditions: Some medications can impact appetite, nutrient absorption, or hydration status. Chronic conditions like diabetes, gastrointestinal disorders, and kidney disease can also influence nutritional health and contribute to falls.
3. Intervention Strategies
- Dietary Adjustments: Ensuring a balanced diet with sufficient protein, calcium, Vitamin D, and other essential nutrients can improve bone and muscle health. Including fortified foods or supplements for nutrients like Vitamin D may be necessary, especially in populations with limited sun exposure.
- Hydration: Encourage adequate fluid intake to prevent dehydration, which can contribute to dizziness and falls.
- Exercise and Physical Activity: In conjunction with proper nutrition, strength training and balance exercises (e.g., Tai Chi, resistance exercises) help improve muscle mass, coordination, and stability.
- Vitamin D and Calcium Supplementation: In cases of deficiency, doctors may recommend Vitamin D and calcium supplements to enhance bone density and reduce fall risk.
- Multidisciplinary Approach: Collaborating with dietitians, physical therapists, and healthcare providers to address both nutritional deficiencies and physical limitations can lead to a more comprehensive fall prevention strategy.
4. Screening Tools for Falls and Nutrition
- Mini Nutritional Assessment (MNA): This tool helps to identify elderly patients at risk for malnutrition by assessing weight loss, dietary intake, and overall health.
- Comprehensive Geriatric Assessment (CGA): Includes evaluations for nutrition, functional capacity, cognitive function, and the risk of falls.
- Timed Up and Go (TUG) Test: This is a mobility assessment often used alongside nutritional evaluations to measure an elderly person’s fall risk by testing their ability to stand up, walk, and sit down.
Anthropometric measures
Body weight
- Body weight is a key indicator of nutritional status.
- The weight history serves as an indicator of nutritional risk.
- Periods of significant weight loss include 2% body weight in a week, 5% in a month, 7.5% in 3 months, and 10% in 6 months.
Height or other estimates of stature
- The height changes are largely due to compression of the spine.
- If unable to stand or stand straight, estimates of stature can be estimated via Arm span, Demi-span, and Knee height.
- Arm span measurements can determine the maximal height in adulthood rather than one’s actual height.
- The race-specific equations are used to estimate stature from knee height measures.
Weight history
Body mass index (BMI)
- BMI of less than 24 is associated with poor nutritional health.
- BMI between 24 and 29 is believed to be a healthy weight.
- BMI of over 29 is seen as overweight and may lead to health problems.
Skinfold thickness
In older adults, skinfold thickness measurements are not reliable measurements.
Circumference
(e.g., waist, waist-to-hip ratio, and upper arm circumference), much like measures that are used to estimate skeletal muscle mass.
Biochemical
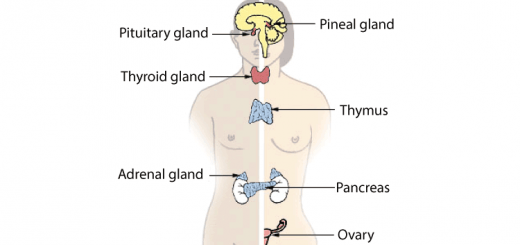
Biochemical markers of visceral protein include:
- serum albumin, thyroxine-binding prealbumin, serum transferrin, and retinol-binding protein as well as total lymphocyte counts.
- serum albumin can predict mortality in older adults, but it is not always reliable. Values can be elevated as a result of dehydration, or values can decline because of inflammation, infection, and age-related degeneration of muscle mass.
Biochemical measures to assess lipid status include: total cholesterol, high-density lipoprotein, low-density lipoprotein, and triglycerides
Biochemical markers for Hematologic assessments include: hemoglobin, hematocrit, mean cell volume, mean cell hemoglobin concentration, mean cell hemoglobin, and total iron binding capacity.
Clinical
The components of clinical assessment can include:
- Medical history.
- Physical signs and symptoms associated with nutritional deficiencies.
Physical Examination
- General look: temporalis/masseter muscles.
- Face: Eyes, Lips, Tongue, Pellagric skin rash.
- Teeth & gums.
- Conjunctival, congestion, Xerosis, Bitot spots.
- Angular stomatitis and Cheilosis.
- Pellagric skin rash.
- HANDS: interosseous muscle wasting, thenar, hypothenar wasting, and pallor (palms).
- NAILS: loss of luster, longitudinal fissuring, and flattening or spooning.
- FOREARM: follicular hyperkeratosis, pellagric rash (pressure points).
Functional status
- Activities of daily living (ADL), which include basic self-care such as bathing, grooming, dressing, feeding, and toileting.
- Instrumental activities of daily living (IADLS), which include cooking, shopping, housekeeping, and managing one’s affairs.
Cognitive status
MMSE (Mini Mental Status Examination)
Dietary factors
Dietary assessment methods can be categorized as:
- A retrospective assessment involves the recall of all foods and fluids consumed in a particular time frame (often 24 hours). Retrospective assessment can be unreliable if the individual has problems with his or her cognitive status.
- A prospective assessment may be favored, as this involves keeping a written record of all foods and fluids consumed in a given period (e.g., 3 days [including 2 weekdays and a weekend day] or 7 days).
Comprehensive assessment of nutritional status is complex and time-consuming. Rapid screening is beneficial to identify those who might be at risk for poor nutrition and individuals who might need in-depth assessment. Several screening tools exist.
Mini Nutritional Assessment (MNA) is used for the initial screening and assessment of individuals in the community as well as in long-term care settings.
Nutrition requirements
- Reduction in energy requirements is one notable difference between individuals older than 65 years of age and their younger counterparts.
- One simple method, only requiring a patient’s weight, estimates energy expenditure in the range of 20 to 25 total kcal/kg/day.
- Energy expenditure in critically ill older adults was found to be 22 to 25 kcal/kg/day.
- If weight gain is the desired objective, an increase in calories up to 30 kcal/kg/day
- For protein, this corresponds to between 10% and 35% of total energy intake.
- Dietary protein intake is recommended at 0.8 g/kg of body weight to maintain protein equilibrium and avoid loss of lean body mass for all adults, regardless of age.
- Evidence suggests as much as 1.0 to 1.2 g of protein/kg of body weight is required to meet the needs of healthy older adults.
- Protein needs for older adults may reach 1.2 to 1.5 g/kg body weight for those with acute or chronic diseases.
- 2.0 g/kg body weight for those with severe infections, surgery, or trauma.
- Patients with existing renal disease should avoid high-protein diets as they may hasten a greater decline in renal function.
- Intake of high-quality protein sources, such as fish, lean meat, dairy products, eggs, and legumes is recommended at each meal throughout the day.
- Ideally, total fat intake should fall within 20% to 35% of total daily energy intake.
- Older adults should acquire 45% to 65% of their daily energy intake from complex carbohydrates, such as whole grains, vegetables, and fruits.
- The adequate intake of fluid is the same for older and younger adults.
- A water intake of 1 ml/calorie ingested or 30 ml/kg/day with a minimum of 1500 ml/day is generally recommended to meet dietary water requirements and achieve adequate fluid intake in older adults
- 1200 mg/day of calcium for women older than 50 years and men older than 70 is essential to protect against decreased absorption of calcium and bone loss.
- Recommendations for vitamin D are 600 IU for individuals aged 51 to 70 and 800 IU for those older than 70.
- Insufficient levels of vitamin B6, in addition to folate and vitamin B12, are known to contribute higher than normal levels of serum homocysteine, a known risk factor in the development of coronary artery disease, stroke, and depression, as well as a decrease in cognitive function.
You can follow science online on YouTube from this link: Science online
You can download Science Online application on Google Play from this link: Science online Apps on Google Play
Aging and cognition, Dementia symptoms, types, What comes first, dementia or Alzheimer’s?
Causes of Falls in the elderly, How to prevent falls and Why the Elderly die after a fall
Urinary incontinence in elderly causes and treatment, How to correct urinary incontinence?
Properties of cardiac muscles, Cardiac automaticity, and Conduction of electrical impulses
Histology of the heart, Cardiomyocyte types, Ultrastructure, and features of cardiac muscle fibers
Mediastinum contents, Aorta parts, Brachiocephalic trunk, Pulmonary trunk, and Thoracic duct trunk
Electrocardiogram (ECG) importance, ECG test results, analysis and abnormalities
Heart function, structure, Valves, Borders, Chambers and Surfaces
Delirium causes, types, diagnosis, treatment, Why do people get delirium and can delirium be cured?