Myocardial infarction cause, signs, types, treatment, and What is myocardial infarction in ECG?
Myocardial infarction is Ischemic necrosis of part of the cardiac muscle due to sudden persistent and complete cessation of its blood supply, A myocardial infarction is a medical emergency that requires immediate attention to minimize heart damage and improve the chances of survival.
Myocardial infarction
A myocardial infarction (MI), commonly known as a heart attack, occurs when the blood flow to a part of the heart muscle is blocked for an extended period, leading to damage or death of the heart tissue. This blockage is usually caused by a buildup of fatty deposits (plaque) in the coronary arteries, which supply blood to the heart. When a plaque ruptures, it can form a blood clot that obstructs the flow of blood, causing an MI.
Symptoms of Myocardial Infarction
- Chest Pain or Discomfort is often described as pressure, tightness, squeezing, or aching in the center or left side of the chest. The pain can radiate to the shoulders, arms, neck, jaw, or back. Often accompanies chest discomfort, and can occur before or without chest pain. Profuse sweating or cold, clammy skin.
- Nausea or Vomiting is a common symptom, especially in women.
- Feeling faint or about to pass out.
- Unusual tiredness, which may be especially prominent in women.
- A feeling of impending doom or panic, similar to a panic attack.
Retrostemal pain. Precordial pain Similar to angina but:
- Pain Associated with fever and tachycardia & associations of angina.
- More severe, it may be severe enough to be described as the worst pain the patient has ever felt.
- More prolonged ≥30m up to several hours.
- Unrelated to exercise: may be at rest.
- Not relieved by rest or sublingual nitrate.
- Radiates more: may be below the epigastric area but never below the umbilicus.
Causes and Risk Factors
Atherosclerosis is the primary cause of Myocardial infarction, where plaque builds up in the arteries, narrowing them and reducing blood flow, Blood clots can form in a narrowed artery, blocking blood flow to the heart muscle.
Coronary Artery Spasm is a temporary tightening of the muscles within the artery walls that can reduce or block blood flow. Risk Factors include smoking, high blood pressure, high cholesterol, diabetes, obesity, lack of physical activity, unhealthy diet, stress, and a family history of heart disease.
Diagnosis
- An electrocardiogram (ECG or EKG) measures the electrical activity of the heart and can identify heart damage.
- Blood Tests: Troponin levels, among other markers, are checked to detect heart muscle damage.
- Echocardiogram: uses sound waves to create images of the heart, showing how it is pumping and where damage may have occurred.
- Coronary Angiography: A dye is injected into the coronary arteries to visualize blockages through X-ray imaging.
Treatment
- Immediate Treatment:
- Aspirin: Reduces blood clotting, helping to keep blood flowing through a narrowed artery.
- Thrombolytics: Drugs that dissolve blood clots.
- Antiplatelet Agents: Prevent new clots from forming.
- Pain Relief: Nitroglycerin or morphine to relieve chest pain.
- Oxygen Therapy: Helps to supply oxygen to the heart.
Procedures
- Percutaneous Coronary Intervention (PCI) is also known as angioplasty, a procedure that opens blocked coronary arteries, It involves placing a stent to keep the artery open.
- Coronary Artery Bypass Grafting (CABG): A surgery where a blood vessel from another part of the body is used to bypass the blocked artery.
Medications
- Beta-Blockers: Reduce the heart’s workload and decrease the chances of another MI.
- ACE Inhibitors: Help relax blood vessels and lower blood pressure.
- Statins: Lower cholesterol levels and reduce the risk of further heart problems.
- Anticoagulants: Help prevent blood clots from forming.
Prevention
- Lifestyle Changes: Quitting smoking, eating a heart-healthy diet, exercising regularly, maintaining a healthy weight, managing stress, and controlling conditions like high blood pressure, diabetes, and high cholesterol are crucial.
- Medications: For those at high risk, medications may be prescribed to manage blood pressure, cholesterol levels, and other risk factors.
Prognosis and Aftercare
- Cardiac rehabilitation programs help individuals recover and prevent future heart problems through exercise, education, and counseling.
- Long-Term Management: Ongoing lifestyle changes and medication adherence are vital for reducing the risk of another MI.
Etiology
- Thrombosis on top of atherosclerosis.
- Coronary embolism (rare).
- Severe coronary spasm.
Types
- STEMI/Q-wave: Transmural infarction (ST-elevation myocardial infarction – STEMI): infarction of full thickness of the ventricular wall.
- NSTEMI/NON-Q-wave: Subendocardial (Non-ST-elevation myocardial infarction-NSTEMI): Transient or incomplete vessel occlusion.
Signs
- S1: weak.
- S2: reversed splitting.
- S3 gallop: due to LVF.
- S4 gallop: due to decreased myocardial compliance.
- Murmur: of MR, (rupture papillary muscles).
- Pericardial rub: Dry pericarditis.
- Fine basal crepitation: MR (lung congestion).
- Congested neck vein: in right ventricular infarction.
Important notes
- The mortality of (MI) in the elderly is higher than in younger people.
- The presenting symptoms of (MI) can be quite atypical, especially in patients over age 80.
- Dyspnea is a very common early manifestation.
- Mental confusion, syncope, gastrointestinal complaints.
- Elderly patients with (MI) have an increased incidence of complications.
- Many patients have conduction defects on the ECG that may mask the changes of acute MI, but elevated specific cardiac enzymes confirm that MI did occur.
Investigations
1. ECG
STEMI:
- ST-segment elevation.
- Reciprocal ST depression.
- Hyperacute T-wave.
- Pathological Q wave.
NSTEMI/NON Q WAVE:
- ST depression/normal.
- Inverted T-wave.
- No pathological Q-wave.
2. Thallium Scintigraphy
(Radioactive Thallium 201) Thallium 201: is taken up by healthy myocardium & not by ischemic myocardium (cold spot).
3. Coronary angiography
reveals which vessels have been affected and the extent of damage. generally used to determine whether mechanical revascularization (CABG or PTCA) is possible & to guide this therapy.
4. cardiac enzymes
troponin elevated.
Cardinal signs of MI
- Suggestive pain > 30 min.
- ECG.
- Increased cardiac enzymes (Elevated cardiac enzymes are serum troponin LDH CKMP).
Treatment
A. Non-medical
- Rapid transfer to hospital is a must (Time lost is lives lost).
- Oxygen inhalation.
B. medical
Thrombolytic therapy (90m)
- The earlier that thrombolytic therapy is given after the onset of chest pain, the greater the benefit (thrombolytic therapy is beneficial for up to 6 hours but may be given for up to 12 hours).
- Tissue plasminogen activator during the first 3 hours of MI is a more effective thrombolytic agent with the potential for less hemorrhagic complication.
- Streptokinase & Alteplase (more effective).
- (Antiplatelet) Full-dose anticoagulation therapy is often given to patients with anterior MI because of the high risk of mural thrombus and possible embolization.
- Pain relieve: Nitroglycerine, morphine.
C. Interventional (30m)
The indication for PTCA or coronary bypass surgery (cabg) after MI in elderly patients depends on the severity of the symptoms. & if thrombolytic therapy failed.
The best treatment is primary PCI (Percutaneous coronary intervention), If PCI is Contraindicated as in left main vessel disease: (CABG) Medically: as treatment of angina in between attacks.
You can follow science online on YouTube from this link: Science online
You can download Science Online application on Google Play from this link: Science online Apps on Google Play
Properties of cardiac muscles, Cardiac automaticity and Conduction of electrical impulses
Histology of the heart, Cardiomyocyte types, Ultrastructure and features of cardiac muscle fibers
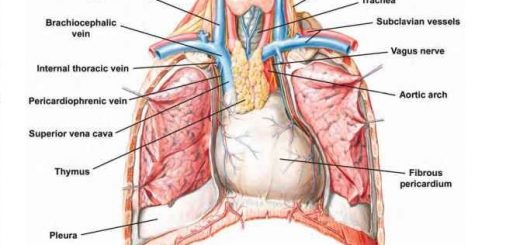
Mediastinum contents, Aorta parts, Brachiocephalic trunk, Pulmonary trunk and Thoracic duct trunk
Electrocardiogram (ECG) importance, ECG test results, analysis and abnormalities
Heart & Pericardium structure, Abnormalities and Development of the heart
Heart function, structure, Valves, Borders, Chambers and Surfaces
Cardiac Markers review, definition, list, test, and myoglobin function