Heart failure causes, signs, stages, treatments and can you survive heart failure?
Heart failure is a clinical syndrome in which the heart can’t maintain adequate cardiac output to meet the body’s metabolic needs despite normal ventricular filling, 6-10% of people older than 65 years have HF.
Heart failure
Heart failure is also known as congestive heart failure (CHF), It is a chronic condition in which the heart‘s ability to pump blood effectively is diminished, leading to inadequate circulation of blood and oxygen throughout the body, This can cause symptoms that affect the quality of life and can be life-threatening if not managed properly.
Precipitating factors
- Infections: chest infections, infective endocarditis.
- latrogenic:
- Calcium channel blocker (- ve inotropic).
- Cortisone (salt & water retention).
- Discontinuation of antifailure therapy.
- Physical & emotional stress.
- Pregnancy & delivery.
- Hyper dynamic circulation.
- Anemia.
- Hyperthyroidism.
- Arrhythmias (tachy & brady arrhythmias).
Left-sided heart failure
Causes
Left ventricular failure: 3 x 3:
- Muscle disease: (systolic heart failure): Myocardial infarction (CAD), Myocarditis, CardioMyopathy.
- Volume (diastolic) overload: (increase preload): Hyperdynamic circulation. (systolic heart failure), Valvular disease: MR, AR, Congenital disease: VSD, PDA.
- Pressure (systolic) overload: (increase after load): Systemic hypertension, Aortic stenosis (calcific degenerative), Coarctation of aorta.
Symptom
Manifestations of (LCOP):
- CNS Dizziness, headache, syncope.
- CVS: Ischemic heart disease.
- Kidney: Oliguria.
- Skin Cold, peripheral cyanosis.
- Skeletal muscle: fatigue, intermittent claudication.
- Blood pressure: low systolic blood pressure.
- Pulse: Weak.
Manifestations of pulmonary congestion backward manifestations):
- Dyspnea: Exertional, orthopnea, paroxysmal nocturnal dyspnea, or dyspnea at rest.
- Exertional Cough.
- Recurrent chest infections.
- Hemoptysis.
- Pleural effusion.
- Pulmonary edema.
Signs
- Bilateral basal crepitation. (bibasilar rales).
- tachypnea.
- chyne stoke respiration.
- expiratory wheezes.
- Pleural effusion (flatness in percussion/decrease or absent breath sound).
Cardiac signs
- Left ventricular enlargement.
- Tachycardia.
- Hypotension and cyanosis.
- Aortic stenosis and mitral regurge.
- Apex displaced downward and laterally.
- Pulsus alternans: alternating strong & weak beats (In the advanced stage).
- Gallop on the apex: due to flabby ventricle.
- murmure of functional MR: pan-systolic murmur due to LV dilatation.
Right-sided heart failure
Right ventricular failure: 3×3
- Muscle disease: The same as left. {systolic heart failure)
- Volume (diastolic) overload: Hyperdynamic circulation (systolic heart failure), Valvular disease: TR, PR, Congenital disease: VSD, ASD
- Pressure (systolic) overload: (systolic heart failure): pulmonary hypertension. (cor pulmonale), pulmonary stenosis, pulmonary embolism.
- Most common cause of RSHF is LSHF.
Symptoms
Manifestations of LCOP:
- CNS: Dizziness, headache, syncope.
- CVS: Ischemic heart disease.
- Kidney: Oliguria.
- Skin: Cold, peripheral cyanosis.
- Skeletal muscle: fatigue, intermittent claudication.
- Blood pressure: low systolic blood pressure.
- Pulse: Weak.
Manifestations of systemic congestion:
- Insomnia.
- Sweating on slight activity: due to sympathetic activation.
- Congested neck vein. /HJR.
- Edema lower limb/sacral odema, later on ascites.
Cardiac Signs: (the same as left without pulsus alternans):
- Right ventricular enlargement.
- Tachycardia.
- gallop (over tricuspid area).
- murmur of functional TR.
Another classification
1. Systolic dysfunction (HFrEF):
is present when the ejection fraction is less than 40% (normal ejection fraction: 55-60%).
- coronary artery disease (most common).
- hypertensive heart disease.
- calcific degenerative aortic stenosis.
- valvular heart disease.
- calcification of the mitral annulus.
- cor pulmonale.
- myocarditis.
- thyroid disease.
- Tachy-or bradyarrhythmias.
- idiopathic (diagnosis of exclusion).
2. Diastolic heart failure (HFpEF):
- 30-50% of patients with CHF have normal LV systolic function.
- These patients may have comorbid conditions accounting for symptoms.
- Diastolic function is often abnormal.
- More prevalent with age.
- More common in females.
- Asymptomatic diastolic dysfunction is more common than symptomatic.
Causes
- Structural Abnormalities: Hypertrophy, Fibrosis, Constriction.
- Functional Abnormalities: Ischemia, Calcium overload, ATP depletion.
3. HFpEF borderline / intermediate 41%-49% EF.
- The incidence of diastolic dysfunction is age-related and heart failure due to diastolic dysfunction rises dramatically with age.
- Mortality rates in heart failure are high even for patients compliant with the best available treatments 50% die within 5 years of diagnosis.
- When heart failure symptoms are stabilised by current treatments, it may seem that patients are doing well, but the neurohormonal imbalance underlying heart failure is still silently occurring, resulting in disease progression.
- All heart failure patients, even those who are considered asymptomatic (NYHA class I) or mildly symptomatic (NYHA class II), are at high risk of dying.
- The neurohormonal imbalance that causes the disease to progress is present in all heart failure patients, even in those who are considered asymptomatic (NYHA class I) or mildly symptomatic (NYHA class II).
- Sudden death is the most frequent cause of cardiovascular (CV) mortality among Systolic heart failure patients.
- 40%of cardiovascular deaths are due to sudden death.
NYHA classification
- Class I: no limitation of physical activity, ordinary physical activity doesn’t cause symptoms.
- Class II: slight limitation of physical activity. comfortable at rest, but ordinary physical activity causes symptoms.
- Class III: marked limitation of physical activity. comfortable at rest but less than ordinary physical activity causes symptoms.
- Class IV: unable to carry out any physical activity without discomfort Symptoms at rest. if any physical activity is undertaken discomfort is increased.
ACCF/AHA Functional classification
- Stage A – At high risk of HF but without structural heart disease.
- Stage B – Structural heart disease without signs or symptoms of HF.
- Stage C – Structural heart disease with prior HF or current HF.
- Stage D-Refractory HF requires special Interventions.
Management
Investigation
1. X-ray
- Increased heart size-cardiothoracic ratio≥ 0.50.
- Large hila with indistinct margins.
- The prominence of superior pulmonary veins;
- cephalization (visualization) of flow.
- Fluid in Interlobar fissures.
- Pleural effusion.
- Kerley’s B lines.
- Alveolar edema.
- Peribronchial cuffing.
2. ECG
- Detect the cause e.g. MI.
- Chamber enlargement.
3. cardiac catheterization
- Chamber enlargement.
- Detect the cause.
4. BNP
B natriuretic peptide :(if normal, HF is unlikely).
Causes of elevated natriuretic peptides
Cardiac:
- Heart failure.
- Acute coronary syndromes.
- Pulmonary embolism.
- Myocarditis.
- Hypertrophic or restrictive cardiomyopathy.
- Left ventricular hypertrophy.
- Valvular heart disease.
- Congenital heart disease.
- Atrial and ventricular tachyarrhythmias.
- Heart contusion.
- Cardioversion, ICD shock.
- Surgical procedures involving the heart.
- Pulmonary hypertension.
Non-cardiac:
- Advanced age.
- Ischaemic stroke.
- Subarachnoid haemorrhage.
- Renal dysfunction.
- Liver dysfunction (mainly liver cirrhosis with ascites).
- Paraneoplastic syndrome.
- Chronic obstructive pulmonary disease.
- Severe infections (including pneumonia and sepsis)
- Severe burns.
- Anaemia.
- Severe metabolic and hormone abnormalities (e.g. thyrotoxicosis, diabetic ketosis).
5. Echocardiography (key investigation)
- Chamber enlargement.
- Detect the cause.
- Paradoxical movement of the myocardium.
- measures COP & Ejection fraction (EF).
Ejection fraction. Systolic volume end-diastolic volume
- N = 50%
- EF < 40% systolic heart failure.
Treatment of CHF due to systolic dysfunction
- Diet.
- Exercise.
- ACE inhibitors and angiotensin II receptor antagonists.
- Diuretics.
- Beta-Blockers.
- Digoxin.
Treatment of CHF due to diastolic dysfunction
- Diet.
- Exercise
- Diuretics
- Other Pharmacologic Considerations.
B-blockers
- Historically, ẞ blockers were contraindicated in HF due to their -ve inotropic effect. (decrease cop).
- Recently: ẞ blockers are indicated in HF because they were found to start with low doses with gradual increase.
- Reduce mortality & improve the prognosis.
- Prevent arrhythmia.
- Decrease blood pressure
- e.g. bisoprolol, Metoprolol, Carvedilol (best).
Diuretics
- They increase salt & water excretion So, decrease the work of the heart.
- Decrease Edema & visceral congestion.
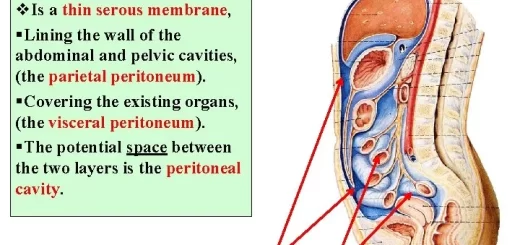
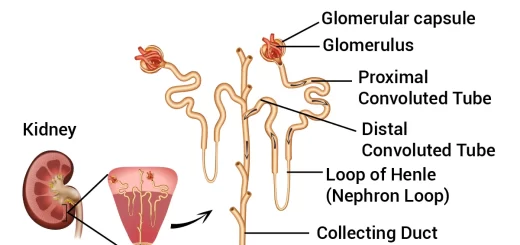
- THIAZIDE: DCT (hypokalemia) is MORE useful in hypertension than edema.
- Furosemide: a loop of Henle (prevent reabsorption of Na & K.
- HYPOKALEMIA. potassium sparing diuretics:e.g. Spirnolactone (aldosterone antagonist) HYPERKALEMIA.
Vasodilators
They are classified into:
- Arteriolar: Reduce afterload, Hydralazine, Diazoxide.
- Venous: Reduce preload, Nitrates.
- Both: Reduce both, ACEIs Na nitroprusside.
ACE inhibitors are the best vasodilator in cases of CHF, especially in LV failure.
Inotropic agents
Digitalis:
- Increase Contractility of the ventricles.
- Increase Excitability.
- Digitalis toxicity (most life-threatening).
- Increase excitability: arrhythmias.
Tips in old
- Older people may show an exaggerated drop in blood pressure after the first dose of an ACE inhibitor.
- Check postural blood pressures frequently and BUN/creatinine ratios at intervals to monitor volume depletion.
- Check serum electrolytes and magnesium and replace when necessary. Digoxin is useful in treating CHF due to systolic dysfunction.
- Many older people will have some reduction in renal function. Therefore, give maintenance doses of digoxin based on creatinine clearance.
- Digoxin toxicity can present atypically in the elderly with headaches and other neurological manifestations.
A 72 year-old man is referred to you because of a precordial systolic murmur. On examination, there is a harsh mid-systolic crescendo-decrescendo murmur at the right parasternal 2nd ICS, radiating to the carotids. The patient is asymptomatic. Echocardiography reveals an aortic valve area of 1.2 cm2 and a mean systolic gradient of 30 mmHg and a normal LV systolic function. What is the most appropriate intervention for this patient at present?
- Percutaneous balloon aortic valvuloplasty.
- Aortic valve replacement.
- Conserve and follow up.
A patient with newly-discovered aortic regurgitation and severe chest pain should be considered to have:
- Myocardial infarction.
- Acute pericarditis.
- Aortic dissection.
- Syphilitic aortitis.
- Ankylosing spondylitis.
You can follow science online on YouTube from this link: Science online
You can download Science Online application on Google Play from this link: Science online Apps on Google Play
Properties of cardiac muscles, Cardiac automaticity and Conduction of electrical impulses
Histology of the heart, Cardiomyocyte types, Ultrastructure and features of cardiac muscle fibers
Mediastinum contents, Aorta parts, Brachiocephalic trunk, Pulmonary trunk and Thoracic duct trunk
Electrocardiogram (ECG) importance, ECG test results, analysis and abnormalities
Heart & Pericardium structure, Abnormalities, and Development of the heart
Heart function, structure, Valves, Borders, Chambers and Surfaces
Cardiac Markers review, definition, list, test, and myoglobin function