Benign prostatic hyperplasia, What is the best treatment for BPH?, How do you reduce BPH symptoms?
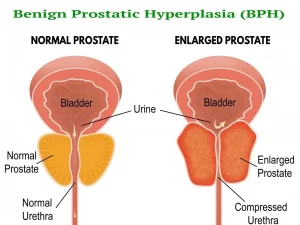
Benign prostatic hyperplasia (BPH) is also referred to as an enlarged prostate, It is a condition in older men where the prostate gland enlarges. As the prostate enlarges, it can squeeze the urethra, causing problems with urination. The exact cause of BPH is unknown, but it’s thought to be related to changes in hormone levels as men age.
Benign prostatic hyperplasia (BPH)
Age: 6th decade. The most common benign neoplasm in the aging male.
Etiology (Risk factors)
A male who:
1. Lives long (longevity, aging process).
2. Have testes (source of p production of testosterone).
- The main circulating androgen in the body is testosterone. 95% is produced from testes and 5% from adrenal glands.
- 95% of circulating androgen is bound to protein (inactive form) while 5% is the free active testosterone.
- Testosterone must be converted to Dihydrotestosterone DHT to pass into the inside of the prostate by an enzyme called 5 alpha-reductase enzyme.
- DHT is controlling metabolism, cell division, and growth of the prostate.
Zones of the prostate
The prostate is anatomically composed of five zones: periurethral, transitional, central, peripheral, and anterior zones.
Site of Origin
BPH arises from the transition zone of the prostate. The transition zone (constitutes only 5% of the prostate volume) is located in the innermost portion of the prostate and is enveloped by the peripheral and central zones from the outside (95% of the prostate volume).
Zones of the prostate
- Transition zone.
- Central zone. Site of origin of infections.
- Anterior fibromuscular zone.
- Peripheral zone. The most common site of carcinomas of the prostate.
Surgical Capsule
The peripheral and central zones are progressively compressed by the BPH growing in the transition zone. They undergo atrophy and form a thin layer that acts as a capsule around the BPH. This is not a true capsule; it is referred to as the “false capsule”. It is also referred to as the “surgical capsule”.
Pathology
1. BPH is composed of fibro-musculo-glandular components: (i) stroma (connective tissue + smooth muscle fibers); and (ii) adenoma (periurethral glands).
The firm consistency of the stromal component + soft consistency of the adenomatous component give BPH a firm elastic (india rubbery) consistency (felt like contracted thenar eminence).
3. Lobes of BPH: 2 lateral lobes on either side of the supramontanal urethra + 1 median lobe behind the supramontanal urethra.
4. The average size of BPH is 20 gm in males below 40 years. It is rarely huge exceeding 200 gm. There is NO correlation between the size of BPH and the intensity of urinary symptoms.
5. There is no correlation between BPH & carcinoma of the prostate. Their simultaneous existence is only a co-incidence.
6. Boundaries of BPH:
- Superiorly: bladder neck.
- Inferiorly: verumontanum.
- Inwards: urothelial lining of the supramontanal urethra.
- Outwards: false (surgical) capsule.
7. Direction of growth of BPH:
Inwards: compression of the lumen of the supramontanal urethra causing obstructive urinary symptoms.
(ii) Posteriorly: backward compression of the anterior rectal wall that is felt by digital rectal examination.
(iii) Upwards: into the bladder in the plane between the bladder urothelium and the internal sphincter muscle. This appears as a basal filling defect in the cystogram.
8. Upward extension of BPH within the internal sphincter causes the sphincter to overstretch around it. The internal sphincter eventually loses its muscle tone and becomes atrophied. This is the reason why the bladder neck is seen patulous after surgical removal of BPH. Post-operative urinary continence becomes dependent only on the external sphincter.
Pathophysiology of obstruction
1. Static component.
- The bulk of the gland (especially with infection, infarction, and congestion)→ elongation, compression, and angulations of the prostatic urethra.
- Middle lobe obstruction of the bladder neck (ball-valve).
- Bladder stones as a complication may obstruct the bladder neck &/or result in irritative LUTs.
2. Dynamic component
Prostatic smooth muscles are innervated by alpha-adrenergic fibers, which increase in the growing BPH leading to increased resting tone in the bladder neck sphincter.
Diagnosis
I. Symptoms:
- Irritative urinary symptoms: frequency (diurnal and nocturnal), possibly with urgency, caused by trigonal irritation from the growing adenoma. There is no burning micturition unless there is a secondary infection (cystitis).
- Obstructive urinary symptoms: hesitancy, difficulty, straining, weak and narrow urine stream, interruption, bifurcation of the urine stream, terminal dribbling, or acute retention if the obstruction is complete Collectively these two sets of symptoms are called LUTS (lower urinary tract symptoms).
- Gross hematuria: occurs earlier than carcinoma of the prostate due to proximity of the transition zone to the urethra. This occurs in enlarged adenomas with rupture of vessels over them (varices).
- Obstructive symptoms occur earlier in BPH than carcinoma due to the same reason mentioned above.
II. Examination
Digital rectal examination: the anterior rectal wall is felt pushed posteriorly by a prostatic swelling firm elastic (India rubbery) in consistency.
III. Investigations
1. Ultrasonography of abdomen & pelvis: Size of the gland, amount of post-voiding residual urine, and possible associated hydro-ureteronephrosis, associated bladder pathology as tumors or stones, diverticula.
2. IVU: Smooth central basal filling defect in the cystogram caused by intravesical enlargement of the prostate. A raised bladder base causes a bilateral fish-hook appearance of the lower end of both ureters.
3. Cystoscopy: direct visualization of BPH, with appropriate estimation of the size and evaluation of the bladder.
4. Uroflowmetry: Simple, non-invasive test to measure the urine flow rate (Q max). Maximum Flow Rate < 10ml/Sec indicates obstruction &/or weak detrusor muscle. The patient voids into a special container connected to the transducer to calculate his maximum flow rate.
5. Laboratory investigations. Include renal function tests and serum PSA. PSA (prostate-specific antigen) is normally 0-4 ng/ml. It could be elevated in any process affecting the prostate, such as prostatitis, or carcinoma, huge BPH, vigorous DRE, ejaculation, prostatic biopsy, cystoscopy, or catheterization.
Complications
- Acute urine retention.
- Chronic retention of urine if the bladder becomes decompensated, with resultant bladder underactivity (weak bladder).
- Upper tract dilatation and uremia and renal failure.
- Cystitis.
- Bladder stones.
- Severe uncontrolled hematuria (rare).
Treatment
1. Watchful waiting: avoid risk factors (weather, work, wine).
2. Medical treatment for mild or moderate symptoms:
- α-adrenergic blockers e.g. alfuzosin, tamsulosin, terazosin, silodosin → relaxation of the bladder neck and BPH smooth muscle fibers, thus widening the urethra. Side effects. Postural hypotension and retrograde ejaculation.
- 5-α-reductase inhibitors e.g. finasteride, dutasteride → inhibit the conversion of testosterone to dihydrotestosterone, causing a decrease in the size and vascularity of the prostate and widening of the urethra. The effect takes 6 months to decrease the size of the prostate by 20%. Side effects: decreased libido, reduced ejaculate volume, and breast tenderness.
- Phosphodiesterase 5 inhibitors (Tadalafil 5mg). It increases the nitric oxide which converts ATP to CAMP causing relaxation of the smooth muscles in the prostate and bladder neck. This drug is originally used in the treatment of erectile dysfunction.
- Phytotherapy: herbal therapy for prostatic congestion symptoms. Combination therapy is the best and most effective, especially in large prostates.
3. Surgical adenectomy for patients with severe symptoms or complications: The surgical procedure is not called prostatectomy. Only the prostatic adenoma is resected and removed, leaving the “prostatic cavity” that is located between the bladder neck and the verumontanum and is lined by the surgical (false) capsule. This could be done in either an open or transurethral endoscopic approach.
- Transurethral resection of the adenoma using the resectoscope (TURP) and electric current.
- Transurethral vaporization of the adenoma using the resectoscope and laser beams.
- Open adenectomy: Retropubic or transvesical approach (open surgery done for huge adenomas that are technically difficult to be removed by the transurethral approaches). Open enucleation of the adenoma from the surgical capsule.
- Permanent suprapubic cystostomy: if patients are not medically fit to undergo surgery; e.g. they suffer from associated severe cardiac disease, stroke, or chronic renal failure,
- Prostatic stent.
Indications of surgical intervention in cases of BPH
- Repeated attacks of acute urinary retention (AUR).
- Bilateral Hydronephrosis and elevated renal functions (chronic urinary retention).
- Recurrent attacks of Hematuria.
- Recurrent urinary tract infection (UTI).
- Bladder stones.
- Severe obstructive symptoms.
- Poor response to medical therapy.
- Side effects of medical treatment.
You can subscribe to Science online on YouTube from this link: Science Online
You can download Science Online application on Google Play from this link: Science Online Apps on Google Play
Benign prostatic hyperplasia (BPH), TRUS biopsy, Prostate disease symptoms and treatment
Enlarged prostate symptoms, Prostatic artery embolization (PAE) importance and risks
Common procedures of Interventional Radiology and the best Interventional Radiologists
Interventional radiology types, Robotic endovascular systems advantages & disadvantages
Cone beam CT vs. Fan beam CT, CBCT advantages, disadvantages & uses
Artificial intelligence in radiology decision support systems, Medical Imaging and Healthcare
Prostate function, structure, lobes, Benign enlargement of prostate and malignant prostatic tumor
Thyroid nodules, Thyroid Fine Needle Aspiration Biopsy importance and risks
Uterine fibroid embolization risks, importance & Minimally invasive procedure specialists