Andrology, What does an andrologist do?, Male infertility causes and Treatment
Andrology is a field of medicine that specifically focuses on men’s health, particularly the male reproductive system and urologic issues that only affect men. It’s essentially the male counterpart to gynecology, which deals with women’s reproductive and urologic health.
Andrology
Andrologists are medical professionals who specialize in diagnosing and treating a variety of conditions, including Infertility, Erectile, dysfunction, Low testosterone levels, Testicular cancer, Peyronie’s disease, and Varicocele. They may also perform procedures such as vasectomies, vasectomy reversals, and testicular biopsies.
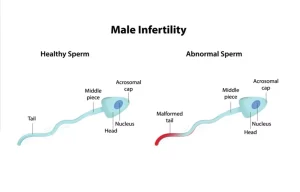
Male infertility
Infertility is the inability of a sexually active, non-contracepting couple to achieve spontaneous pregnancy within one year.
Incidence
- 15% of couples do not achieve pregnancy within one year and seek medical- treatment for infertility.
- 50% due to factors. female factor, 30% due to male factor, 20% due to combined factors.
Risk factors
Pre-testicular: Endocrine disturbances: hypopituitarism, hypothalamic abnormalities.
Testicular:
- Increased scrotal temperature (e.g. as a consequence of varicocele).
- Genetic abnormalities: Sertoli cell-only syndrome and Klienfilter syndrome.
- Testicular malignancy.
Post-testicular:
- Obstructed vas or epididymis.
- Urogenital tract infections.
- Absent vas or ligated vas.
Diagnosis
1- History taking: infertility history, sexual history, medical history, surgical history, drug history, environmental history and occupational history.
2- Physical examination: testicular examination, epididymal examination, presence of the vas deferens, varicocele, digital rectal examination, and inguinal scars.
3. Laboratory evaluation:
A. Semen Analysis: at least two tests.
- Oligospermia: < 15 million spermatozoa/mL.
- Asthenospermia: < 32% progressive motile a spermatozoa.
- Teratospermia: < 4% normal forms.
- Azospermia: Absent spermatozoa.
B. Hormonal profile: FSH, LH, Prolactin, and Testosterone.
4- Imaging:
- Doppler scrotal ultrasound: to assess the testicular size, epididymis, varicocele, tumors…..etc.
- Trans-rectal ultrasound: to assess seminal vesicles and cystic lesions which may cause obstruction.
Types
1. Oligoasthenoteratospermia (OAT syndrome).
2. Azospermia:
- Obstructive
- Non-obstructive.
Treatment
Medical treatment
1) Specific treatment
a. Replacement hormonal therapy in case of endocrinal abnormalities. eg HCG for hypogonadism.
2) Empirical treatment:
- Antioxidants.
- Supplements including zinc.
- Antiestrogens.
- Steroids.
- Pentoxyfylline.
Surgical treatment
- Testicular biopsy in suspected obstructive azospermia.
- Varicocelectomy in oligo-athen-teratospermia.
- Vasovasostomy in obstructed vas.
- Transurethral incision (TUI) of ejaculatory ducts if there is proven ejaculatory duct obstruction by a cyst.
Erectile dysfunction (ED)
Persistent inability to attain and/or maintain an erection sufficient to permit satisfactory sexual performance for at least three months. Although ED is a benign disorder, it may affect physical and psychosocial health and may have a significant impact on the quality of life of p patients and their partners.
Incidence
52% of adult males aged 40-70 years (mild to severe ED).
Anatomy and physiology of erection
The Penile shaft consists of 3 cylindrical structures – paired corpora cavernosa and corpus spongiosum (which surrounds the urethra) – covered by a loose subcutaneous layer and skin.
- Upon sexual stimulation, there is a release of neurotransmitters from the cavernous nerve terminals (mainly nitric oxide) which leads to the relaxation of smooth muscles and the following events:
- Arterial & arteriole dilatation increased blood flow into the expanding sinusoids… ..erection.
- Venous compression – reducing venous outflow.
- sinusoidal relaxation and stretching of the tunica to its capacity – occludes the emissary veins and further decreases the venous outflow to a minimum…..rigid erection.
- The relaxation of the smooth muscle of the penis relies on the parasympathetic nervous system. The sympathetic nervous system controls ejaculation and also causes constriction of smooth muscle. This constricts the blood-containing lacunar spaces of the penis and empties them of blood, therefore aiding detumescence (subsiding from sexual arousal).
Parasympathetic stimulation leads to erection while sympathetic stimulation leads to detumescence. sexual stimului might be: visual, olfactory, imaginary or tactile.
Risk factors
- Psychogenic: including stress and psychic disorders (high sympathetic tone).
- Arteriogenic: due to vascular anomalies e.g. atherosclerosis.
- Venogenic: due to venous leakage (secondary to arterial insufficiency)
- Neurogenic: DM, & post radical pelvic surgery.
- Hormonal: mostly in hypogonadism with low testosterone levels or hyperprolactinemia.
- Systemic diseases: including hypercholesterolemia, DM, obesity, metabolic syndrome, and smoking.
- Drugs: e.g. antiandrogens, antipsychotics, antihypertensives & H2 blockers.
Diagnosis
1) History taking:
- Medical history: vasculogenic, neurogenic, hormonal, and psychological disorders.
- Sexual history (onset, duration, circumstances…..).
2) Physical examination:
- Genitourinary: Peyronie’s disease, small testis, DRE.
- Neurological (peripheral neuropathy).
- Vascular especially peripheral pulsations.
- Endocrinal (gynecomastia, body built & hair growth).
3) Laboratory investigations:
- Hormonal: testosterone, prolactin.
- Lipid profile.
- Fasting blood sugar and postprandial sugar level.
- Rarely: thyroid function tests.
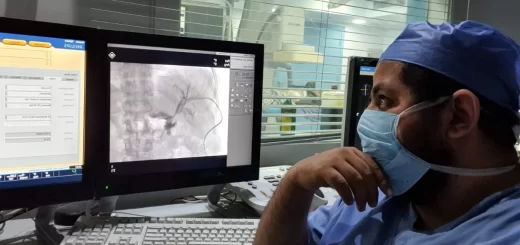
4) Imaging:
Penile Doppler: to assess arterial and venous pathways.
5) Other tests (office based): Intracavernous injection test: via injecting a vasoactive drug intracorporeally and assess the erectile status.
Treatment:
1) Correct modifiable causes: e.g Psychotherapy, stop smoking, treat DM, weight loss, and stop causing drugs.
2) Pharmacotherapy:
a. Oral drugs: Phosphodiesterase 5 inhibitors (PDESIs) e.g. Sildenafil, Tadalafil, Vardenafil: these groups of drugs increase blood flow in the erectile tissue via increasing sinusoidal relaxation.
Intracavernous injection: alprostadil, papaverine, phentolamine.a Prostaglandins.
3) Vacuum erection devices: provide passive engorgement of the corpora cavernosa, together with a constrictor ring placed at the base of the penis to retain blood within the corpora.
4) Other non-invasive restorative therapy:
- Low-intensity shock wave therapy to promote vascularity.
- Stem cell therapy.
5) Penile prosthesis (last line of treatment): The surgical implantation of a penile prosthesis is indicated only in:
- Patients who do not respond to all the above lines of treatment.
- Patients who prefer a permanent solution to their problem.
The two currently available classes of penile implants include inflatable (2 and 3-piece) and malleable devices.
You can subscribe to Science online on YouTube from this link: Science Online
You can download Science Online application on Google Play from this link: Science Online Apps on Google Play
Benign prostatic hyperplasia (BPH), TRUS biopsy, Prostate disease symptoms and treatment
Enlarged prostate symptoms, Prostatic artery embolization (PAE) importance and risks
Prostate function, structure, lobes, Benign enlargement of prostate and malignant prostatic tumor
Nephroblastoma (Wilm’s tumor), Risk factors of Urothelial tumors (Tumors of transitional epithelium)
Urinary bladder structure, function, Control of micturition by Brain and Voluntary micturition
Urinary system structure, function, anatomy, organs, Blood supply and Importance of renal fascia
Histological structure of kidneys, Uriniferous tubules & Types of nephrons